2022's Monkeypox Outbreak: Everything You Need to Know
| 07/12/22
By continuing to use our site, you agree to our Privacy Policy and Terms of Use.

There is increasing concern about the growing monkeypox outbreak of 2022 but for many, the disease is still a bit of a mystery. How do you get it? Is there a vaccine or treatment options available? Who is most at-risk?
Ever since people initially dismissed COVID-19 as something serious and ended up surprised by the never-ending pandemic that followed its outbreak, many are trying to get ahead of the monkeypox outburst of 2022 before it’s too late. Despite the fact that the monkeypox virus, or MPV, isn’t necessarily a “gay virus,” it has impacted a significant portion of gay and bi men globally.
As such, it is important to break down what MPV is, how it spreads, how it can be avoided, and how it can be treated if one does acquire an infection. Thankfully, science is way ahead of treating and understanding MPV in comparison to COVID-19, which is ultimately great news.
Monkeypox, or MPV, is a viral disease with symptoms that include rashes, red blisters, and swollen lymph nodes. This disease was first identified in animals in the 1950s but has since mutated to affect humans as well. In people, MPV can cause fever and other flu-like symptoms during its infection period, typically followed by painful rashes on the body. According to the World Health Organization, MPV has a fatality rate that ranges from zero to 11 percent.

Some publications have linked the current outbreak to certain Pride gatherings taking place in Europe. But just like any other virus, MPV is not exclusive to the LGBTQ+ community. However, it has primarily affected gay and bi men during this 2022 resurgence. According to the Centers for Disease Control and Prevention, there are 351 confirmed cases of MPV in the United States as of this writing — the largest numbers being 80 in California, 72 in New York, 46 in Illinois, and 35 in Florida.

The CDC has listed a few main methods of transmission for MPV: “direct contact with the infectious rash, scabs, or body fluids; respiratory secretions during prolonged, face-to-face contact, or during intimate physical contact, such as kissing, cuddling, or sex; touching items (such as clothing or linens) that previously touched the infectious rash or body fluids; pregnant people can spread the virus to their fetus through the placenta.” In other words, MPV can be transmitted between sexual partners and/or by simply touching someone’s body or belongings if that person has been infected. However, it is not found in semen or vaginal secretions, so condom use will not prevent transmission.
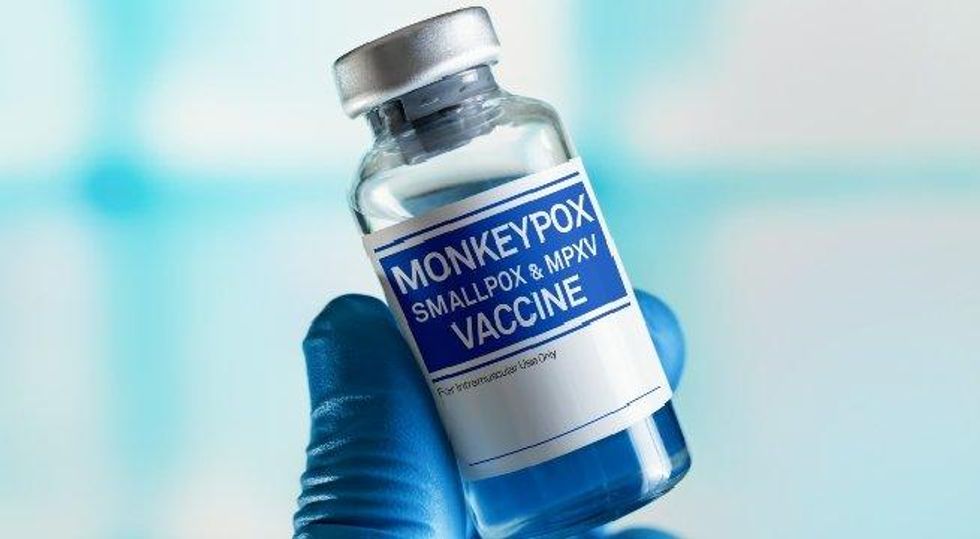
Fortunately, this new outbreak isn’t starting from zero when it comes to treatment and prevention options, which was one of the main problems associated with the COVID-19 pandemic. Overall, the CDC has noted that “because [the] monkeypox virus is closely related to the virus that causes smallpox, the smallpox vaccine can protect people from getting monkeypox. Past data from Africa suggests that the smallpox vaccine is at least 85 percent effective in preventing monkeypox.” Thus, for the time being, smallpox vaccines are being administered with a high success rate for preventing transmission of the virus or assuring that if the recipient still contracts it, their symptoms will be less severe.
The federal government Tuesday announced an expansion of vaccine distribution. If someone does contract MPV, it usually subsides within two to four weeks and can be managed with pain medication. But more severe cases may call for treatment with TPOXX, a prescription drug that is also used against smallpox. People with weakened immune systems due to HIV or other causes are at risk for severe symptoms.