Treatment GuideJust DiagnosedSex & DatingAfrican AmericanStigmaAsk the HIV DocPrEP En EspañolNewsVoicesPrint IssueVideoOut 100
CONTACTCAREER OPPORTUNITIESADVERTISE WITH USPRIVACY POLICYPRIVACY PREFERENCESTERMS OF USELEGAL NOTICE
© 2026 Pride Publishing Inc.
All Rights reserved
All Rights reserved
By continuing to use our site, you agree to our Privacy Policy and Terms of Use.
With the creation of his five-year, $15 billion international AIDS budget, President Bush has established an unprecedented commitment to battling the pandemic. But while the U.S. coffers may soon overflow for those suffering abroad, a relatively dry well remains for HIV-positive individuals at home. In his budget, presented in January, the president requested a $100 million increase for the AIDS Drug Assistance Program. But even with such a hike, it is estimated that the 56 state and territorial ADAPs will suffer a $283 million shortfall in the 2004 fiscal year. Not since ADAPs nearly collapsed into bankruptcy after the introduction of protease inhibitors in 1996 has their solvency picture been more clouded. As of June, 15 ADAPs had restricted access to care or capped enrollment, which had forced over 500 applicants onto waiting lists. Six additional states report they expect to impose new or additional program restrictions in the next fiscal year, according to the National Alliance of State and Territorial AIDS Directors. And it is not just the little guys who are feeling the pinch anymore. Even New York has begun to reduce its vast formulary, and other major programs are considering restrictions for the first time. Michael Montgomery, chief of the California Department of Health Services Office of AIDS, boils down the dilemma to the most simple financial formula: 'If we want to avoid restrictions on access, we're going to have to both limit our expenditures and increase our revenues.' Budget increases may prove elusive, although advocates are pressuring Congress for an emergency supplemental appropriation for ADAP. But costs can come down, according to various experts who weighed in for HIV Plus on how to save a program that since 1987 has provided lifesaving medications to lower-income Americans with HIV and that has over 135,000 members. Make Someone Else Pick Up the Tab Federal guidelines prohibit patients who are eligible for any other form of insurance from receiving ADAP drug benefits. One exception: As an alternative to prescription coverage, ADAPs are allowed to pay for health care premiums in outside plans or to subsidize copayments or deductibles, though not all state programs do so. Many state ADAPs insist they have instituted stringent procedures to identify patients who could receive their drug coverage on someone else's dime. Florida, for example, has developed a successful computerized database of its members to cross-reference them for other forms of insurance eligibility. Yet, according to Thomas P. McCormack, public benefits policy consultant at the Title II Community AIDS National Network, the comparable efforts of most states to ensure that an applicant has exhausted all insurance resources still fall short. He points out that while about 18,000 U.S. veterans receive HIV care from the Department of Veterans Affairs, a VA official estimated in 2000 that there are probably thousands of VA-eligible vets using ADAP. Unfortunately, HIV-positive vets frequently shy away from VA care because they wrongly assume they are ineligible or because they have unfounded fears that they will be rejected for homosexuality or drug use. McCormack says ADAPs do an inadequate job of identifying such cases. He also says that while ADAPs ask about eligibility for private insurance, this question often does not yield an accurate response. This is because the low-income applicants either consider the insurance they can obtain to be far too expensive and do not consider it an option or they are unaware they are eligible as a dependent, most notably when they do not know they qualify for a domestic-partner benefit. McCormack cites a 1999 report from the Center for Studying Health System Change showing that 19% of the Americans in poverty who have access to employer-sponsored health insurance are still uninsured, primarily because of cost. McCormack says ADAPs need to conduct a more thorough search in order to weed out these applicants and possibly subsidize their premiums. Paying for patient premiums instead of for their medications promises to produce significant savings. According to a 2000 study conducted by the Health Resources and Services Administration, the average monthly cost savings per patient of purchasing a new policy was $390, or 50%; and paying to continue an old policy saved $506, or 65%. Yet in 2002 only $18.5 million'or 2% of the national ADAP budget'was used to pay for insurance purchase and maintenance, with 5,272 clients covered as of June of that year. Another way ADAPs can cash in on their status as the last resort is through their right to collect retroactive payments from other insurers that should have been paying for the patient all along. According to the National ADAP Monitoring Project's annual report, released in April, ADAPs recouped $14.5 million through 'insurance recovery' in 2002. One of the report's authors, Jennifer Kates, director of HIV policy at the Henry J. Kaiser Family Foundation, says insurance recovery 'is one of these things that should be happening.' Acknowledging that recouping these losses is cumbersome, she predicts that ADAPs will begin to attempt to do so on a broader level as their budget crises become more dire. Reduce the Cost of Drugs ADAPs are already able to negotiate significant reductions in the cost of pharmaceuticals, thanks to their inclusion in a federal program known as 340B. Before this program was created in its current form in 1992, drug manufacturers had a disincentive to offer major discounts to drug assistance programs because Medicaid discount levels are based on national averages of drug sale prices. If the average price goes down, then so do drug companies' sales receipts from Medicaid. The 340B statute exempted its members from this calculation (within certain parameters), in turn giving them greater leeway to obtain discounts similar to Medicaid's. Of the 49 ADAPs that participate in 340B, 26 use independent pharmacy networks to distribute the drugs and then obtain rebates afterward. The remaining 23 ADAPs purchase drugs directly on discount and then must self-distribute the drugs through a state public-health infrastructure or mail order. A 2000 report from the Office of the Inspector General at the Department of Health and Human Services found that, in general, direct-purchase programs yield significantly lower drug prices. The report recommended that HRSA encourage states to switch from the rebate model. But the study acknowledged that the issue is far from cut-and-dried. Direct-purchase states must cope with the additional overhead to distribute the drugs, and traveling to a county health department rather than to the local Walgreen's presents an access challenge for patients. Nevertheless, William E. Arnold, director of the ADAP Working Group, says many states are considering the switch-over, and he thinks states should evaluate their status every few years'in case a revision could yield cost savings. In the same publication the OIG reported that ADAPs could have saved $72 million in 1999 if they were allowed to purchase 10 antiretrovirals at the 'federal ceiling price''a steep level of discount available only to certain federal agencies. Also, while 340Bs have a ceiling price above which manufacturers cannot sell them medications, there is no floor, so drug companies have a strong disincentive to allow subceiling price discounts, because at that point the sale is no longer exempt from the Medicaid price calculation. In the report, the OIG pressured HRSA to change both these regulations, but three years hence, the laws remain the same. In March a scandal erupted when the OIG reported that five drug companies had overcharged 340B programs, including ADAPs, by $6.1 million. (The drugmakers were not identified.) According to William von Oehsen, counsel to the Public Hospital Pharmacy Coalition, it is nearly impossible to have independent oversight over fair 340B pricing because the two national averages on drug discounts that pharmaceutical companies use to set the sales prices are both confidential to anyone but the Center for Medicaid Services and the drug companies. As the OIG conducts a study of the problem, Von Oehsen recommends that the agency conduct regular inspections and that ADAPs demand better efforts to ensure fair pricing. In a sign of a new era of uniquely collective vigilance, eight of the largest state ADAPs formed the ADAP Crisis Task Force earlier this year to bargain on behalf of all ADAPs with the eight U.S. manufacturers of anti-HIV drugs over lowering their prices. All the companies have agreed to price freezes and greater rebates, for an estimated annual savings of $65 million. Montgomery attributed this success in part to the fact that with a 25% share of the national anti-HIV drug market, ADAPs possess a unique strength in bargaining power, since drug companies have a vested financial interest in keeping the programs healthy. Make Use of Current Developments A final internal change that experts predict can yield savings is the use of drug resistance testing, which is currently offered by 44% of ADAPs. 'Proper resistance testing is bound to reduce some mistakes'mistakes in terms of the [highly active antiretroviral therapy] regimen you put together'that can easily be classified as wasted money,' says Arnold. And on the forefront is a promise that Medicaid will soon provide expanded care to HIV-positive Americans'and this would be entitlement funds, rather than discretionary. The Early Treatment for HIV Act is wending its way through Congress. 'We have a shot' at passage, says Robert Greenwald of Harvard Law School. Currently, only people who are disabled by HIV disease qualify for Medicaid coverage, although ineligible patients can obtain an individual waiver in some cases. The act would give states the option to include these predisabled low-income HIV-positive applicants in Medicaid, which would in turn shift patients away from ADAP. Admittedly, these myriad solutions are patchwork and cannot promise to change the facts that people with HIV disease are living longer, drug prices continue to skyrocket, and the national economy remains in a state of limbo. However, they do point out that a closer evaluation of the system could make a difference for states with overburdened budgets'and ultimately for HIVers' lives.
From our Sponsors
Most Popular
“So much life to live”: Eric Nieves on thriving with HIV
September 03 2025 11:37 AM
The Talk: Beyond the exam room
August 13 2025 3:15 PM
Messenger RNA could be the key to an HIV vaccine — but government cuts pose a threat
August 20 2025 8:02 AM
It’s National PrEP Day! Learn the latest about HIV prevention
October 10 2025 9:00 AM
Amazing People of 2025: Javier Muñoz
October 17 2025 7:35 PM
The lab coat just got queer
August 21 2025 10:00 AM
The Talk: Owning your voice
August 25 2025 8:16 PM
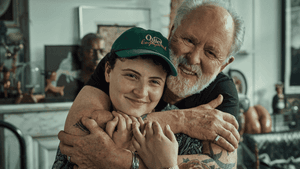
“I am the steward of my ship”: John Gibson rewrites his HIV narrative
September 16 2025 2:56 PM
Plus: Featured Video
Latest Stories
HIV-positive men stage 'Kiss-In' protest at U.S.-Mexico border
December 01 2025 12:56 PM
What the AIDS crisis stole from Black gay men
December 01 2025 6:00 AM
The Talk: Navigating your treatment
August 01 2025 6:02 PM
The Talk: Starting the conversation
July 25 2025 4:47 PM
Thanks to U=U, HIV-positive people can live long, happy, healthy lives
July 25 2025 2:37 PM
How the Black AIDS Institute continues to fill in the gaps
July 25 2025 1:06 PM
“I felt like a butterfly”: Niko Flowers on reclaiming life with HIV
July 23 2025 12:22 PM
Dancer. Healer. Survivor. DéShaun Armbrister is all of the above
July 02 2025 8:23 PM
BREAKING: Supreme Court rules to save free access to preventive care, including PrEP
June 27 2025 10:32 AM
1985: the year the AIDS crisis finally broke through the silence
June 26 2025 11:24 AM
VIDEO: A man living with HIV discusses his journey to fatherhood
June 10 2025 4:58 PM
Trump admin guts $258 million in funding for HIV vaccine research
June 03 2025 3:47 PM
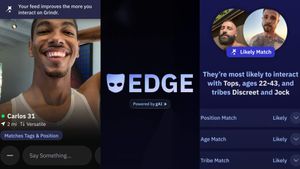
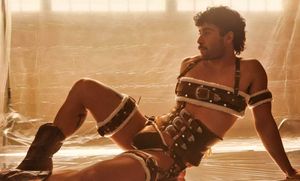
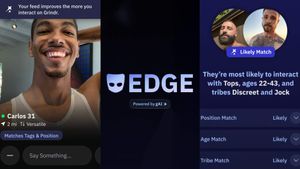
Grindr is reminding us why jockstraps are so sexy and iconic
May 02 2025 5:36 PM
HRC holds 'die-in' to protest Trump health care cuts
April 28 2025 2:11 PM
Two right-wing Supreme Court justices signal they may uphold access to PrEP and more
April 21 2025 4:10 PM
500,000 Children at Risk: PEPFAR Funding Crisis
April 08 2025 3:51 PM