Treatment GuideJust DiagnosedSex & DatingAfrican AmericanStigmaAsk the HIV DocPrEP En EspañolNewsVoicesPrint IssueVideoOut 100
CONTACTCAREER OPPORTUNITIESADVERTISE WITH USPRIVACY POLICYPRIVACY PREFERENCESTERMS OF USELEGAL NOTICE
© 2026 Pride Publishing Inc.
All Rights reserved
All Rights reserved
By continuing to use our site, you agree to our Privacy Policy and Terms of Use.
As most health care providers have come to realize, providing quality medical care to people with HIV is both an art and a science. Treating people with HIV requires a physician to be well-versed in CD4-cell counts, viral loads, more than 20 different HIV medications'and the side effects associated with them. It involves knowing how to properly monitor a person on therapy and determine when a drug regimen should be changed. And it necessitates keeping up to date on all the latest research findings. Advocates have long claimed that access to an HIV specialist could mean the difference between life and death. And research bears this out. Studies have found that the patients seen by doctors with the most experience treating HIV live longer than those seen by doctors with less expertise. In 2000, acting on these research findings, the California state legislature passed a bill requiring health maintenance organizations to offer all HIV-positive patients standing referrals to physicians certified as HIV specialists. It took until January 2003, though, for the law to go into effect after physicians and medical groups hammered out a definition of what constitutes an HIV specialist. Virtually everyone agrees that the law has had a significant impact. 'The health plans have opened up their networks to more HIV specialists as a result,' says Michael Weinstein, president of AIDS Healthcare Foundation, a nationwide specialized HIV medical provider and a major backer of the bill. Yet it is unlikely that any other state will pursue similar legislation. As Weinstein explains, the law 'was of particular importance in California because of the high HIV incidence rate.' There are an estimated 110,000 to 125,000 HIV-positive people in California'about 55,000 of whom are living with AIDS. This was also important in California, Weinstein continues, 'because it is the state with the most managed care' cases. Just under half of the people in the state are enrolled in an HMO. But for states with fewer people with HIV and fewer people in managed care, such legislation would carry little weight. Jane Cheeks, MPH, Alabama's AIDS director, agrees that similar legislation would have little effect in her state. There are about 12,000 people living with HIV in Alabama, she says, and 'about 90% are uninsured.' These patients as well as those who do have insurance see HIV specialists at one of the nine clinics in the state that specifically treat people with HIV disease. Similarly, in Wyoming, where only 2.1% of the state's population is enrolled in an HMO, 'managed care wouldn't be an issue,' says Tonya Cain, executive director of the Wyoming AIDS Project. Cain adds that in Wyoming, which has a population of 500,000, fewer than 200 people are living with HIV, and there are two doctors in the state that see the majority of them. Because other states have fewer people with HIV covered by managed care, the larger issue nationally, Weinstein says, is working to get HIV care accepted as a subspecialty by the medical profession. And toward that end, he says, 'we still have a long way to go.' 'It is important that people get care from people who are well-trained,' says Stephen Boswell, MD, executive director at Fenway Community Health in Boston. 'My overall sense is that the very fact that this legislation was pushed in California helped to raise the issue overall nationally. As a result, there is now a movement toward trying to develop some form of recognition for a specialized qualification for HIV.' But this movement is far from cohesive. There is currently no universal agreement on what constitutes an HIV specialist'as the nearly three years it took experts in California to agree on a definition underscores. In addition, not only does each of the two key players in this arena'the American Academy of HIV Medicine and the HIV Medicine Association'have its own definition, but each is pursuing different strategies for credentialing HIV specialists. The American Academy of HIV Medicine, an independent organization of HIV specialists, initiated a credentialing process for HIV specialists in December 2001. To date, says R. Scott Hitt, MD, founder of the group, about 1,700 doctors, nurse practitioners, and physician assistants have been credentialed. 'Hundreds of clinics nationwide use this as a benchmark to recognize who is qualified to be seen as an HIV specialist,' Hitt says. To receive the credential, which must be renewed ever two years, health care providers must pass a take-home exam that tests their knowledge of HIV treatment issues. 'Life-and-death mistakes can be made if providers are not keeping up to date,' Hitt says. 'And you can't assume that just because a person is seeing a lot of patients that he or she is up to date. We had a provider with more than 100 [continuing medical education] hours, who sees 400 patients, fail the exam.' The HIV Medicine Association, which was created within the Infectious Diseases Society of America in 2000 for all medical professionals engaged in HIV medicine, is working with the American Board of Internal Medicine to allow internists and family practitioners who are not certified in infectious disease to be credentialed as HIV specialists. 'This certification would involve specialized training and sitting for a proctored exam,' says Christine Lubinski, executive director of the HIV Medicine Association. The exam, which would differ from the exam created by the American Academy of HIV Medicine, would be developed by the American Board of Internal Medicine and be certified in conjunction with the American College of Graduate Medical Education. 'We think credentialing should come from organized medicine,' Lubinski says, 'rather than from an advocacy group creating its own credentials.' But this credential is unlikely to be available soon. Not only must the proposal weave its way through a series of committee and board approval processes at the different medical specialties, but a training program would have to be developed and an exam written. This means, Lubinski says, that the earliest this credentialing could go into effect would be 2006. Both groups are in agreement that the issue of quality care needs to be addressed not just by HMOs but by those who care for the uninsured. To that end, Hitt says, his organization is 'trying to get language included in [the] Ryan White [Comprehensive AIDS Resources Emergency Act, a federal AIDS funding law that needs to be reauthorized in 2005] that would ensure access to quality care.' And the HIV Medicine Association, Lubinski says, 'is working to get its definition of an HIV specialist adopted by Medicare and Medicaid programs to ensure quality care for people with HIV seen through those programs.' Not all states have such criteria in place. In the interim, advocates will continue to educate patients and health care providers about the need for HIV specialists and to place increased demands on the medical profession as a whole to tackle this issue. 'I'd like to see the medical profession recognize that many studies show a correlation between outcomes and having knowledgeable providers,' says Weinstein. 'This is not primarily an issue that needs to be addressed by the government. California took the bull by the horns and got legislation passed. But what we need now is to get the medical profession to recognize this and move on it.'
From our Sponsors
Most Popular
“So much life to live”: Eric Nieves on thriving with HIV
September 03 2025 11:37 AM
The Talk: Beyond the exam room
August 13 2025 3:15 PM
Thanks to U=U, HIV-positive people can live long, happy, healthy lives
July 25 2025 2:37 PM
Messenger RNA could be the key to an HIV vaccine — but government cuts pose a threat
August 20 2025 8:02 AM
It’s National PrEP Day! Learn the latest about HIV prevention
October 10 2025 9:00 AM
“I felt like a butterfly”: Niko Flowers on reclaiming life with HIV
July 23 2025 12:22 PM
The Talk: Starting the conversation
July 25 2025 4:47 PM
The lab coat just got queer
August 21 2025 10:00 AM
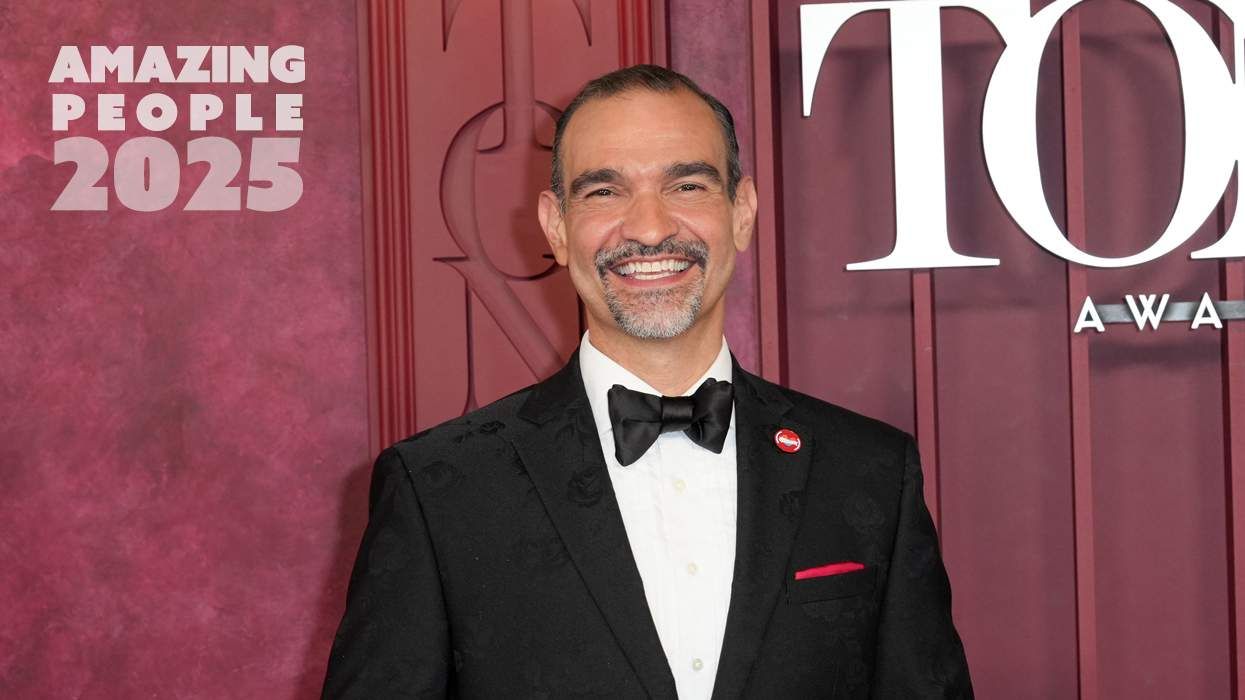
Amazing People of 2025: Javier Muñoz
October 17 2025 7:35 PM
Plus: Featured Video
Latest Stories
HIV-positive men stage 'Kiss-In' protest at U.S.-Mexico border
December 01 2025 12:56 PM
What the AIDS crisis stole from Black gay men
December 01 2025 6:00 AM
“I am the steward of my ship”: John Gibson rewrites his HIV narrative
September 16 2025 2:56 PM
The Talk: Owning your voice
August 25 2025 8:16 PM
The Talk: Navigating your treatment
August 01 2025 6:02 PM
How the Black AIDS Institute continues to fill in the gaps
July 25 2025 1:06 PM
Dancer. Healer. Survivor. DéShaun Armbrister is all of the above
July 02 2025 8:23 PM
BREAKING: Supreme Court rules to save free access to preventive care, including PrEP
June 27 2025 10:32 AM
1985: the year the AIDS crisis finally broke through the silence
June 26 2025 11:24 AM
VIDEO: A man living with HIV discusses his journey to fatherhood
June 10 2025 4:58 PM
Trump admin guts $258 million in funding for HIV vaccine research
June 03 2025 3:47 PM
Grindr is reminding us why jockstraps are so sexy and iconic
May 02 2025 5:36 PM
HRC holds 'die-in' to protest Trump health care cuts
April 28 2025 2:11 PM
Two right-wing Supreme Court justices signal they may uphold access to PrEP and more
April 21 2025 4:10 PM
500,000 Children at Risk: PEPFAR Funding Crisis
April 08 2025 3:51 PM
Broadway's best raise over $1 million for LGBTQ+ and HIV causes
April 03 2025 7:15 PM
The Talk Season 5 premieres this spring with HIV guidance for the newly diagnosed
March 26 2025 1:00 PM