Treatment GuideJust DiagnosedSex & DatingAfrican AmericanStigmaAsk the HIV DocPrEP En EspañolNewsVoicesPrint IssueVideoOut 100
CONTACTCAREER OPPORTUNITIESADVERTISE WITH USPRIVACY POLICYPRIVACY PREFERENCESTERMS OF USELEGAL NOTICE
© 2025 Pride Publishing Inc.
All Rights reserved
All Rights reserved
By continuing to use our site, you agree to our Privacy Policy and Terms of Use.
Vanessa Johnson ought to know better. The soft-spoken 48-year-old has been around the block enough times to figure out what's up. She's battled booze, stumbled through bad relationships, and fought off an all-too-clearly related HIV infection for 16 years. And she is, after all, a senior staffer at the National Association of People With AIDS. So she understands why folks would expect her to be an ideal patient--the sort of person who's engaged in her care, takes her meds correctly, and does what's necessary to support her immune system's tussle with the virus. If only it were so. 'I am not a good patient. I am not adherent. If I go to my doctor visits, I go because something in me said, You need to go and deal with this. So I'm surprised and amazed that I'm here,' Johnson admits. 'I either have a strong constitution or a strong God.' Perhaps both. Nevertheless, Johnson knows she's not unique. Ever since combination therapy revolutionized AIDS treatment in the mid 1990s, doctors and researchers have fretted over how to ease both the fraught decision of whether to start treatment and the hard work needed to succeed in it. The drugs may be scientific wonders, but they don't work on their own, and for many the taxing process of fighting side effects, balancing diets, and keeping up with a pill-popping routine is simply too much. 'I'm the average HIV-positive person,' Johnson says, 'who is scared to death and doesn't know what to do. I take it day by day.' But Johnson's challenges may be all the more typical because she is black. There's little hard evidence, but many doctors and patient advocates believe the treatment reluctance she describes is particularly profound among the more than half a million African-Americans now estimated to be living with HIV. It is certainly clear that blacks have fared far less well than others since the beginning of the combination therapy era, where a racial death gap has existed since the beginning: 1996 was significant not merely because it was the first year in which death rates went down (by a whopping 25% in the United States) but also because it was the first year in which more blacks died than whites. In 2004 nearly twice as many blacks died of AIDS as whites, and today HIV-positive African-Americans are eight times more likely to die of AIDS than their white counterparts. To be sure, the reasons for this gap are myriad and complex. AIDS is certainly not the only disease in which racial disparities persist. From diabetes to asthma, African-Americans not only get preventable illnesses at disproportionate rates but also are more likely to become disabled and die as a result. And as with other diseases, most analysts believe the AIDS disparities are at least in part due to having less access to quality care. Nearly two thirds of blacks in treatment depend on increasingly cash-strapped Medicaid and Medicare programs, while more than four in 10 whites obtain their treatment through private insurance; nearly a quarter of blacks under care are uninsured altogether, compared to 17% of whites. The Centers for Disease Control and Prevention says the death gap is also caused by late testing. The agency estimates that more than a quarter of all HIV-positive African-Americans are undiagnosed. While medical debate over how early one should start antiretroviral treatment remains heated, it's clear that waiting until you get sick steeply reduces the chances of success. So those hordes of undiagnosed infections, the CDC says, mean that too many black people are unwittingly waiting for their immune systems to collapse before starting treatment. The feds have heeded their own warning and launched a massive HIV testing drive in response. But the late testing may itself be part of a larger set of barriers that aren't so easily hurdled. Doctors and patient advocates working with large black client loads point to an interlocking jumble of fear and distrust--directed at both the providers and the medicines themselves--that makes even the most well-informed patients wary of antiretroviral treatment. This trepidation is born from experience. 'The first issue that always comes up,' says Atlanta's Edith Biggers, MD, 'is that we have to talk about mistrust. And it doesn't help that I'm a black woman.' Researchers have focused on conspiracy theories about AIDS as a root cause of that distrust. And studies show that black Americans indeed smell a rat when it comes to this epidemic. In a 2005 RAND Corp. survey, more than half of black respondents said they believe an AIDS cure is being deliberately withheld from poor people and that 'a lot of information' is being hidden from the public. More than a quarter of African-Americans in the survey said they believe 'AIDS was produced in a government laboratory,' and 16% said it was made specifically to control the black population. But Biggers says these sorts of beliefs are actually indicators of broader--and justified--feelings among African-Americans that the health care system isn't actually that interested in black people's well-being. 'It's how you're taken care of on a day-to-day basis,' she explains. 'Patients who go to the public hospital across the street from my office are disrespected and not asked questions about what's happening to them. I have many patients who have had surgery, and they can't even tell me why they've had it.' These sorts of belittling experiences inside the health system both fuel skepticism about AIDS treatment and, just as important, reinforce a passive posture toward one's own health care. 'And that has to be discussed with my patients,' Biggers says, 'before we can even talk about whether or not you're willing to go on [combination therapy] or what your lab numbers actually mean.' Dallas internist Keith Rawlings, who has spent years leading education efforts for physicians working with black HIV patients, adds that the conspiracy conversation itself is a frustrating distraction for him and his patients. 'I get more and more folks coming in wanting to talk to me about Tuskegee,' he says, referring to the infamous decades-long syphilis study involving black men in rural Alabama. 'But they don't even know what happened in Tuskegee,' he complains. Like many people, his patients usually believe that black men were deliberately infected with syphilis; in actuality, government researchers withheld treatment from men already infected with the sexually transmitted disease in order to study its progression in the body. 'So what you're telling me,' Rawlings says to patients who raise Tuskegee as a reason not to start AIDS treatment, 'is you want me to reproduce Tuskegee by not treating you.' Rawlings's experience reinforces the fact that AIDS myths thrive on misinformation. And in that regard they can be traced to the failure Biggers describes: too many providers' unwillingness to meaningfully engage African-Americans about health care in general. Richard Anderson, a peer counselor at Atlanta's AIDS Survival Project, says his introduction to living with HIV came in just such a scenario. He tested positive at a Veterans Administration hospital in Atlanta in 1998. 'I got a phone call at home, and the person was saying, 'You are HIV-positive. You need to get in here right away because I have this medicine you need to take,' ' he recalls, his voice crackling with resentment at the jarring memory. Anderson, a 46-year-old who is now in treatment, says the experience turned him into what some consider a 'problem patient,' but he adds, 'I believe that it works better for me when I have all the information I need in order to make an informed decision. And going into my doctor's office and being rushed to make a decision--I just find that challenging.' Award-winning journalist and HIV Plus contributing editor LeRoy Whitfield, who died of AIDS-related complications in October 2005, wrote regularly in his Native Tongue column about his torment over whether he should initiate antiretroviral therapy. In July 2005, when he was experiencing severe fatigue and went to his doctor, he wrote, 'She told me that if I would stop being stubborn and take meds, I would experience a boost and feel much better. But no matter what I complain about--lack of sex, overdue rent, swollen joints, bunions, Michael Jackson--that seems to be her answer for everything. And that feels more like a measure of control than the honesty that I depend on her for.' If cramming choices down patients' throats spurs rebellion for people like Anderson and Whitfield, it nurtures the opposite in someone like Johnson, who describes her relationship to her care as 'passive.' It's a posture she's long rested on. 'Most of my life I have not made my own decisions--when I was going to have sex, when I was going to start drinking. All the important decisions that you make, they were not decisions I made,' Johnson plaintively confesses, groping for an answer as to why she finds it so hard to do things others consider basic to survival. 'So I never knew how to make those decisions, how to make correct choices. Even at the age that I am--almost 50--I am still having difficulty doing that.' For Johnson, just getting up the will to show up at her doctor's office and state her needs is a challenge; to show up and admit weakness or failure or, worse, to contradict the perspective of someone wielding such uniquely intimate power as one's physician is unthinkable. As HIV-positive activist and writer Keith Green puts it, 'If we are not empowered people in our everyday lives'we will not adhere. We will not make decisions for ourselves. We will not question our doctors. We will not do what we need to do because we don't have day-to-day empowerment in our lives.' These anxieties are made all the more wrenching by the brutal realities of AIDS treatment. Starting on meds is no small matter for many people. As anyone who's been on antiretroviral therapy will testify, even patients who manage the exacting dietary and dosing schedules often get tripped up by the side effects. They are by now legendary: nausea, muscle pain, skin problems, and hair loss--even nerve damage. Patients of all races and backgrounds struggle with these challenges, and drugmakers are frantically trying to come up with new meds that tamp down the side effects and ease dosing schedules. One side effect that docs treating black patients say stands out as a barrier is lipodystrophy, or fat redistribution. Antiretroviral patients often lose fat in their limbs and face, creating a sunken-cheek and spindly-legged look. Some then in turn get fat buildups in the back of their necks or abdomens. Time and again, say black docs, patients who either experience lipodystrophy or hear about it from others flat out reject treatment. 'What I see,' Rawlings says, 'is individuals who are extremely conscious of how their bodies look and as a result will make alterations to or not take therapies based on that. I see this in both men and women in African-American communities, and I see it overwhelmingly among women.' This is more than mere vanity, explains Harvard Medical School's Bisola Ojikutu, MD, MPH. 'People don't want to be stigmatized, and you can tell when somebody has lipodystrophy,' she notes. 'That's a huge issue.' But the recurring theme for physicians and patients alike is control--and who has it. Ultimately, conversations about treatment and its success or failure return to one idea--that be it stigma or side effects, distrust or fear, treatment won't work until patients take control of their lives. For many, that's an elusive prize. 'I love life. I love living,' Johnson unflinchingly declares. 'But I have to say that it's a struggle. And for most of the people I've been involved with who are HIV-positive, it is a daily struggle of acceptance of living with this illness. It is a daily struggle of learning to take care of yourself in a different manner than you have done in the past.'
From our Sponsors
Most Popular
BREAKING: Supreme Court rules to save free access to preventive care, including PrEP
June 27 2025 10:32 AM
Thanks to U=U, HIV-positive people can live long, happy, healthy lives
July 25 2025 2:37 PM
The Talk: Beyond the exam room
August 13 2025 3:15 PM
Plus: Featured Video
Latest Stories
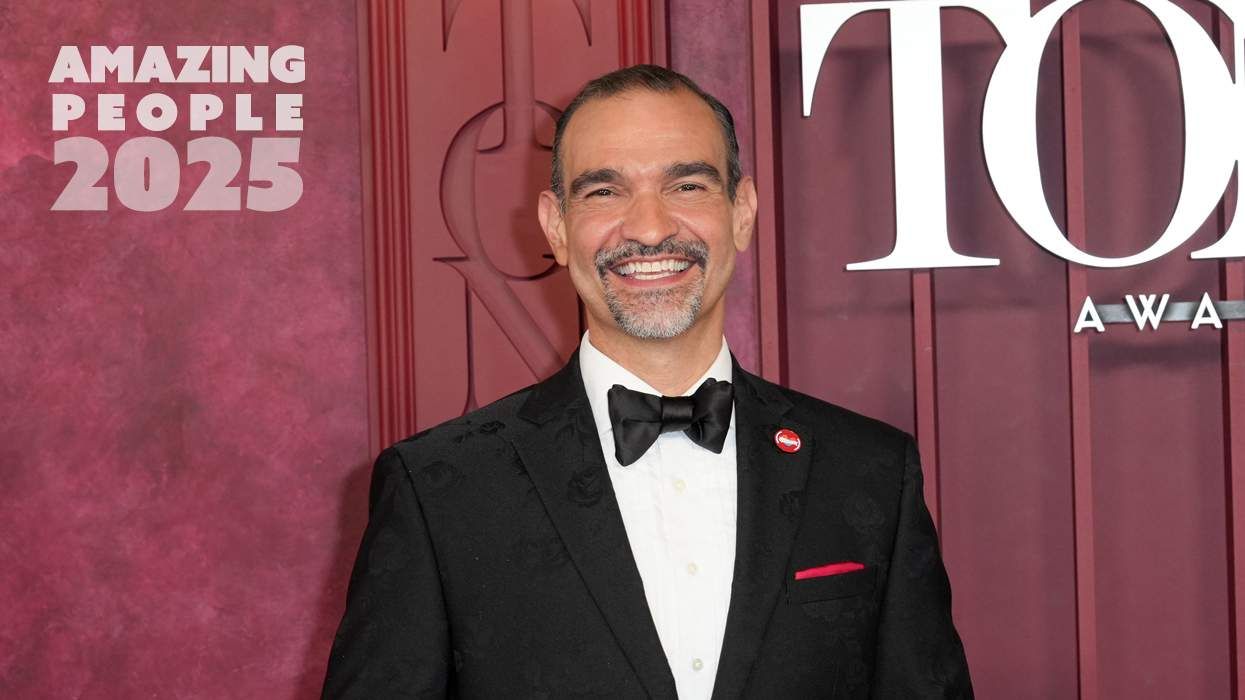
Amazing People of 2025: Javier Muñoz
October 17 2025 7:35 PM
It’s National PrEP Day! Learn the latest about HIV prevention
October 10 2025 9:00 AM
“I am the steward of my ship”: John Gibson rewrites his HIV narrative
September 16 2025 2:56 PM
“So much life to live”: Eric Nieves on thriving with HIV
September 03 2025 11:37 AM
The Talk: Owning your voice
August 25 2025 8:16 PM
The lab coat just got queer
August 21 2025 10:00 AM
Messenger RNA could be the key to an HIV vaccine — but government cuts pose a threat
August 20 2025 8:02 AM
The Talk: Navigating your treatment
August 01 2025 6:02 PM
The Talk: Starting the conversation
July 25 2025 4:47 PM
How the Black AIDS Institute continues to fill in the gaps
July 25 2025 1:06 PM
“I felt like a butterfly”: Niko Flowers on reclaiming life with HIV
July 23 2025 12:22 PM
Dancer. Healer. Survivor. DéShaun Armbrister is all of the above
July 02 2025 8:23 PM
1985: the year the AIDS crisis finally broke through the silence
June 26 2025 11:24 AM
VIDEO: A man living with HIV discusses his journey to fatherhood
June 10 2025 4:58 PM
Trump admin guts $258 million in funding for HIV vaccine research
June 03 2025 3:47 PM
Grindr is reminding us why jockstraps are so sexy and iconic
May 02 2025 5:36 PM
HRC holds 'die-in' to protest Trump health care cuts
April 28 2025 2:11 PM
Two right-wing Supreme Court justices signal they may uphold access to PrEP and more
April 21 2025 4:10 PM