Treatment GuideJust DiagnosedSex & DatingAfrican AmericanStigmaAsk the HIV DocPrEP En EspañolNewsVoicesPrint IssueVideoOut 100
CONTACTCAREER OPPORTUNITIESADVERTISE WITH USPRIVACY POLICYPRIVACY PREFERENCESTERMS OF USELEGAL NOTICE
© 2025 Pride Publishing Inc.
All Rights reserved
All Rights reserved
By continuing to use our site, you agree to our Privacy Policy and Terms of Use.
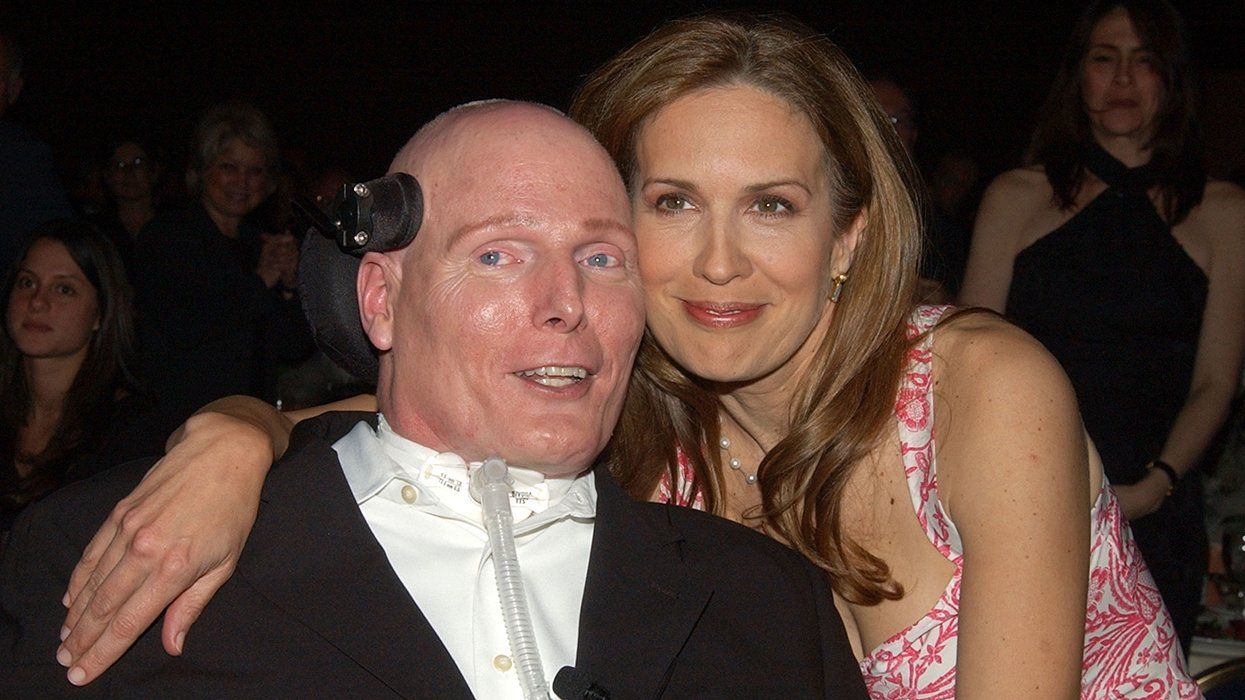
When the Food and Drug Administration announced its approval of Atripla'the first single-tablet triple-drug combination therapy'a year ago it ushered in a new era of simplified regimens. The efforts of thousands are to thank for helping to push the evolution of HIV care toward this important milestone. A vital factor in this fight has been HIVers who have participated in clinical trials since the 1980s and helped to bring the different classes of antiretrovirals to reality. What Is a Clinical Trial? Before gaining approval from the FDA, any medication, lab test, or medical procedure used to treat HIV'or any other disease'must undergo rigorous testing to ensure both its safety and efficacy. Human drug trials are divided into four phases. Phase I, which can last up to a few months, is used to establish preliminary safety data, how the drug is metabolized, and how well it targets HIV. Lasting roughly a year, Phase II better establishes the safety and efficacy of the drug and also studies potential side effects. Phase III weighs the risks and benefits of taking the drug and further studies side effects, safety, and efficacy. If this phase is successful, the drug goes before the FDA to seek approval. This step can take two to three years. Phase IV allows for ongoing research regarding an approved drug's safety and efficacy. There is also an expanded-access phase. During Phase III, if the drug company deems it safe to do so, the FDA allows patients outside the study to take the drug before it is approved. There are roughly 30 new antiretrovirals currently in clinical trials, with many more in the preclinical pipeline. If you're interested in getting involved, there are pros and cons to consider. What Is the Benefit?Finding a potentially effective drug that isn't available yet. This is a particular draw for multidrug-resistant patients who are seeking new drug classes. One such person is activist Nelson Vergel. Last year the 23-year veteran of HIV disease entered a Phase III trial of Merck's MK-518, an integrase inhibitor, along with Prezista, a protease inhibitor available in expanded access that has since been approved by the FDA. He achieved an undetectable viral load for the first time, and his CD4 count jumped from 180 to 440. 'I am so excited,' he says, almost gushing. Keeping an effective therapy in your regimen. If the investigational drug proves to be a useful therapy for you, there is a strong possibility you will be able to remain on it indefinitely. If not, the research team will help you find a new drug regimen. 'We don't let anyone float in the wind,' says Michelle Simek, community education coordinator for the AIDS Research Alliance. 'We will definitely help someone find additional medical care.' Getting access to free medical care and medications. In addition to prescribing meds at no cost, the research team will provide many basic checkup services, such as monitoring blood pressure, weight, CD4 count, and viral load. If you have a primary care physician, it's like adding a layer of care. If you don't have one, the team will try to help set you up with one or even take on that role. Getting access to top-of-the-line tests. Trials often provide regular resistance tests, which are expensive and covered only once a year by most insurers. Pharmacokinetic tests, which analyze how the body is processing meds, are also possible. Receiving one-on-one care from experts. The research team is likely composed of HIV specialists, and they often have the luxury to spend focused time with you'in contrast to the hurried office visits typical of primary care docs. Contributing to the greater good. By participating in a clinical trial, you are participating in the larger effort to improve HIV care for everyone. To provide the best possible safety data for different ethnicities, for example, researchers need diversity in their study populations. Getting a financial incentive. Some studies pay the participants who complete them. What Is the Downside?Facing unknown side effects and safety issues. There is a chance of experiencing unpleasant or even dangerous side effects from an investigational drug. Before consenting to participate, ask what kind of safety nets are in place in the event of adverse reactions. Receiving an ineffective therapy. A drug might not work for you. Taking on a strict schedule. You might have to spend a considerable amount of time visiting researchers' offices. Potentially losing out financially. Ask what expenses'such as travel, parking, and child care'the study will reimburse. New Jerseyan Annette Lizzul paid her way to Boston once a week to participate in an ultimately unsuccessful stem cell research project. Receiving a placebo. In placebo-controlled studies a percentage of participants will receive an inactive sugar pill instead of the drug that is under investigation. Studies should have a provision to move participants on to the active agent if their health begins to decline. Ultimately, after weighing both the pros and the cons, many HIVers who are eager or desperate for new treatments find that they can benefit from participating in a clinical trial.
From our Sponsors
Most Popular
BREAKING: Supreme Court rules to save free access to preventive care, including PrEP
June 27 2025 10:32 AM
“So much life to live”: Eric Nieves on thriving with HIV
September 03 2025 11:37 AM
Thanks to U=U, HIV-positive people can live long, happy, healthy lives
July 25 2025 2:37 PM
The Talk: Beyond the exam room
August 13 2025 3:15 PM
Messenger RNA could be the key to an HIV vaccine — but government cuts pose a threat
August 20 2025 8:02 AM
Plus: Featured Video
Latest Stories
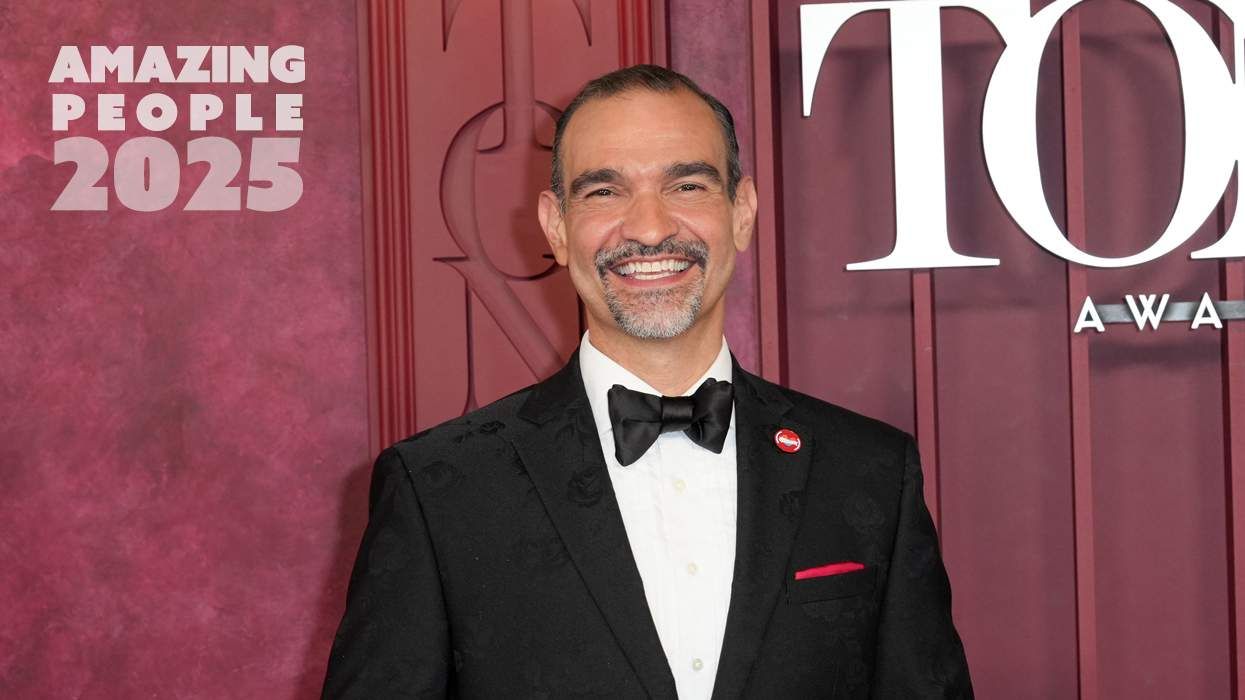
Amazing People of 2025: Javier Muñoz
October 17 2025 7:35 PM
It’s National PrEP Day! Learn the latest about HIV prevention
October 10 2025 9:00 AM
“I am the steward of my ship”: John Gibson rewrites his HIV narrative
September 16 2025 2:56 PM
The Talk: Owning your voice
August 25 2025 8:16 PM
The lab coat just got queer
August 21 2025 10:00 AM
The Talk: Navigating your treatment
August 01 2025 6:02 PM
The Talk: Starting the conversation
July 25 2025 4:47 PM
How the Black AIDS Institute continues to fill in the gaps
July 25 2025 1:06 PM
“I felt like a butterfly”: Niko Flowers on reclaiming life with HIV
July 23 2025 12:22 PM
Dancer. Healer. Survivor. DéShaun Armbrister is all of the above
July 02 2025 8:23 PM
1985: the year the AIDS crisis finally broke through the silence
June 26 2025 11:24 AM
VIDEO: A man living with HIV discusses his journey to fatherhood
June 10 2025 4:58 PM
Trump admin guts $258 million in funding for HIV vaccine research
June 03 2025 3:47 PM
Grindr is reminding us why jockstraps are so sexy and iconic
May 02 2025 5:36 PM
HRC holds 'die-in' to protest Trump health care cuts
April 28 2025 2:11 PM
Two right-wing Supreme Court justices signal they may uphold access to PrEP and more
April 21 2025 4:10 PM
500,000 Children at Risk: PEPFAR Funding Crisis
April 08 2025 3:51 PM