Treatment GuideJust DiagnosedSex & DatingAfrican AmericanStigmaAsk the HIV DocPrEP En EspañolNewsVoicesPrint IssueVideoOut 100
CONTACTCAREER OPPORTUNITIESADVERTISE WITH USPRIVACY POLICYPRIVACY PREFERENCESTERMS OF USELEGAL NOTICE
© 2025 Pride Publishing Inc.
All Rights reserved
All Rights reserved
By continuing to use our site, you agree to our Privacy Policy and Terms of Use.
For people living with HIV, antiretroviral medications have been shown to be effective in preventing progression to AIDS and in improving their quality of life. But these same meds used to treat HIV infection have another benefit; they can be given to an HIV-negative individual who has been exposed to HIV, either through a high-risk sexual or needle-sharing exposure. This type of treatment is called nonoccupational postexposure prophylaxis, or nPEP. For example, if an HIV-positive person has sex with someone who is negative and a condom breaks, the person exposed should be offered antiretrovirals. In fact, giving someone nPEP can reduce the partner's chances of becoming HIV infected by up to 80%! There are two key points that people need to know about nPEP. For one, the quicker that one starts the therapy after the exposure, the more likely nPEP is going to work. The Centers for Disease Control and Prevention says that nPEP is still likely to work for up to 72 hours after the exposure occurred. But one should not wait that long to make the decision or to tell his or her partners to seek care. Every hour that goes by increases one's chances of becoming infected. The other key point that is important to remember is that nPEP needs to be taken for 28 days. Many people who start nPEP do not complete the full 28-day course and thus are less likely to prevent HIV infection. The choice of which meds to give depends on several factors. In New York, for example, we typically give Combivir and Viread. However, if the HIV-positive person that exposed the person has a drug-resistant virus, we typically change the regimen to something that the HIV-positive person's virus is sensitive to. Sometimes that can mean giving someone a lot of meds, including a protease inhibitor or some of the newer drugs used to treat HIV. Oddly, people who are HIV-negative seem to not tolerate these meds as well as people that are HIV-positive, and for that reason it is important to follow patients during their month-long therapy. Although nPEP has been available for almost a decade, very few people know about it or have ready access to the meds. One reason for this is that many doctors and hospitals have been slow to pick this up and are concerned that offering nPEP to people will increase unsafe sex and drug use. Also, many patients feel embarrassed or awkward about asking their providers about nPEP. But every person has a right to the treatment. And nPEP should also be discussed with every HIV-positive patient as a prevention tool in the event of a high risk exposure with someone who is negative or whose serostatus is unknown. Urbina is an HIV specialist and the medical director of HIV education and training at St. Vincent's Comprehensive HIV Center as well as an associate professor of medicine and an associate professor of clinical public health at New York Medical College.
From our Sponsors
Most Popular
“So much life to live”: Eric Nieves on thriving with HIV
September 03 2025 11:37 AM
The Talk: Beyond the exam room
August 13 2025 3:15 PM
Thanks to U=U, HIV-positive people can live long, happy, healthy lives
July 25 2025 2:37 PM
BREAKING: Supreme Court rules to save free access to preventive care, including PrEP
June 27 2025 10:32 AM
Messenger RNA could be the key to an HIV vaccine — but government cuts pose a threat
August 20 2025 8:02 AM
“I felt like a butterfly”: Niko Flowers on reclaiming life with HIV
July 23 2025 12:22 PM
Dancer. Healer. Survivor. DéShaun Armbrister is all of the above
July 02 2025 8:23 PM
The Talk: Starting the conversation
July 25 2025 4:47 PM
The lab coat just got queer
August 21 2025 10:00 AM
Plus: Featured Video
Latest Stories
HIV-positive men stage 'Kiss-In' protest at U.S.-Mexico border
December 01 2025 12:56 PM
What the AIDS crisis stole from Black gay men
December 01 2025 6:00 AM
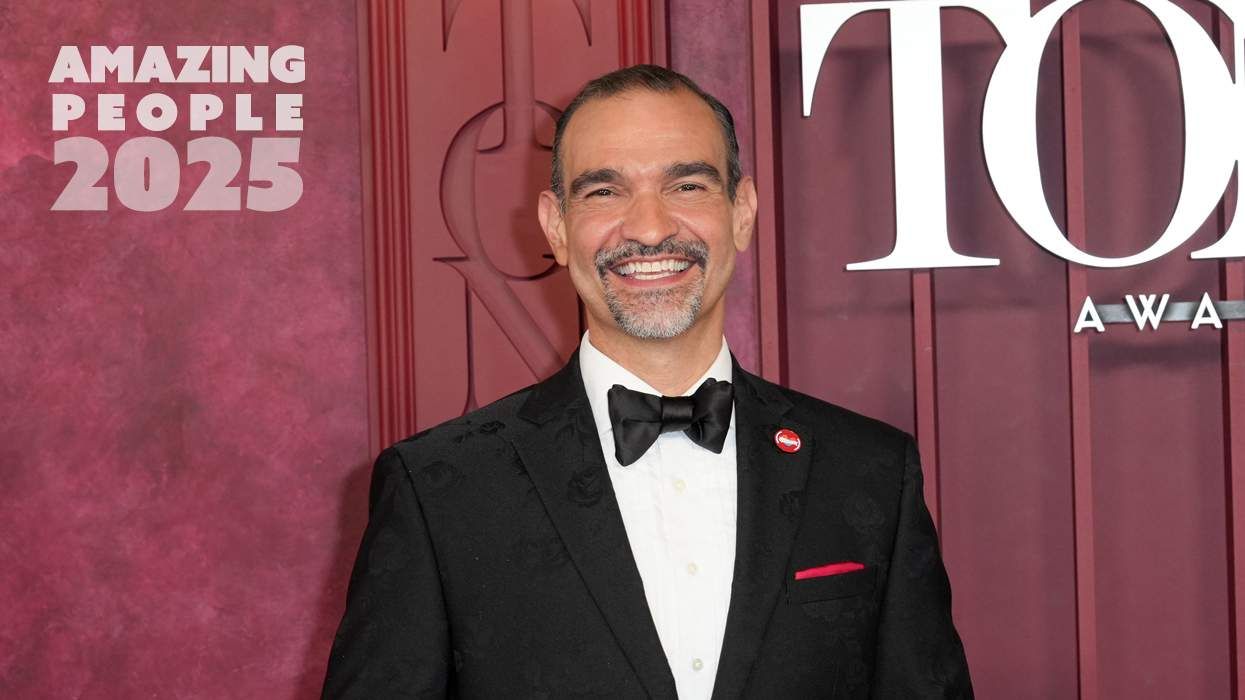
Amazing People of 2025: Javier Muñoz
October 17 2025 7:35 PM
It’s National PrEP Day! Learn the latest about HIV prevention
October 10 2025 9:00 AM
“I am the steward of my ship”: John Gibson rewrites his HIV narrative
September 16 2025 2:56 PM
The Talk: Owning your voice
August 25 2025 8:16 PM
The Talk: Navigating your treatment
August 01 2025 6:02 PM
How the Black AIDS Institute continues to fill in the gaps
July 25 2025 1:06 PM
1985: the year the AIDS crisis finally broke through the silence
June 26 2025 11:24 AM
VIDEO: A man living with HIV discusses his journey to fatherhood
June 10 2025 4:58 PM
Trump admin guts $258 million in funding for HIV vaccine research
June 03 2025 3:47 PM
Grindr is reminding us why jockstraps are so sexy and iconic
May 02 2025 5:36 PM
HRC holds 'die-in' to protest Trump health care cuts
April 28 2025 2:11 PM
Two right-wing Supreme Court justices signal they may uphold access to PrEP and more
April 21 2025 4:10 PM
500,000 Children at Risk: PEPFAR Funding Crisis
April 08 2025 3:51 PM
Broadway's best raise over $1 million for LGBTQ+ and HIV causes
April 03 2025 7:15 PM
The Talk Season 5 premieres this spring with HIV guidance for the newly diagnosed
March 26 2025 1:00 PM
Trending stories
Recommended Stories for You