Treatment GuideJust DiagnosedSex & DatingAfrican AmericanStigmaAsk the HIV DocPrEP En EspañolNewsVoicesPrint IssueVideoOut 100
CONTACTCAREER OPPORTUNITIESADVERTISE WITH USPRIVACY POLICYPRIVACY PREFERENCESTERMS OF USELEGAL NOTICE
© 2026 Pride Publishing Inc.
All Rights reserved
All Rights reserved
By continuing to use our site, you agree to our Privacy Policy and Terms of Use.
Treating hivers with anti-retroviral therapy can reduce the risk of their transmitting the virus to sexual partners by roughly 92%, according to a study published in the medical journal The Lancet. 'These results are an important finding in the search for effective HIV-prevention strategies and the strongest evidence to date that antiretroviral therapy might decrease HIV-transmission risk,' says Connie Celum, a professor of medicine and global health at the University of Washington, located in Seattle. The findings were part of the Partners in Prevention study, a six-year effort coordinated by the International Clinical Research Center at the University of Washington and funded by the Bill & Melinda Gates Foundation. More than 3,400 heterosexual couples in which only one partner had HIV were enrolled from seven African countries. At the beginning of the study, the HIV-infected members had high CD4-cell counts and were not on anti-HIV treatment. Couples were provided counseling and prevention services and were followed for up to two years, with regular CD4 measurements as well as being given treatment referrals when they became eligible for them. During the study, 349 of the HIVers started treatment at an average CD4-cell count of 198. Of the 103 HIV infections that occurred in the couples, there was only one HIV transmission after treatment initiation. In that single event the HIV-infected partner had started antiretroviral therapy about three months prior to HIV infection being first detected in her partner. Deborah Donnell, the study's lead author and a biostatistician with the Vaccine and Infectious Disease Institute at the Fred Hutchinson Cancer Research Center in Seattle, says, 'The one transmission indicated that HIV-serodiscordant couples should maintain safer-sex practices even when HIV-positive partners are on treatment.' And in fact, the proportion of couples who reported having unprotected sex decreased over time, according to the study, and the couples received frequent counseling on HIV risk reduction. Although the rate of new HIV infections has been declining worldwide, an estimated 7,400 people a day are being infected with HIV, according to the Joint United Nations Programme on HIV/AIDS. More than 60 million people have been infected with HIV since the pandemic began. AIDS-related complications are the leading cause of death in sub-Saharan Africa and are the fourth leading cause of death globally. 'Our analysis of HIV-discordant couples indicates that the risk of HIV transmission is significantly lower after HIV-infected people initiate antiretroviral therapy,' Celum says. She notes that a randomized trial is under way to determine the longer-term impact of antiretroviral meds on transmission of the virus. 'While awaiting those results,' she adds, 'our study indicates that initiation of antiretroviral therapy may have a significant public-health benefit as well as clinical advantages for the individuals being treated.' Antiretroviral therapy is known to decrease the concentration of HIV in blood plasma to low levels, the authors explain, likely making the individual less infectious to others. Viral suppression to very low levels was achieved in 70% of individuals in this study at an average of seven months after starting treatment. Transmission occurred at all CD4-count levels. However, since transmission risk was highest among people with CD4 counts less than 200 and not on treatment, findings from this observational cohort indicate that the effect of anti-HIV therapy on prevention of transmission could be greatest in people with CD4-cell counts less than 200. Additionally, the investigators found that among HIV-infected individuals with CD4 counts above 200, transmission rates were highest among those with a viral load above 50,000, suggesting that targeting this group could be an effective way to achieve further transmissions of the virus. This study suggests that starting HIVers on antiretroviral therapy ' even late in the disease ' has benefits for the individual and HIV prevention. While there is movement to initiate treatment earlier for clinical benefits and increasing recognition of the potential HIV-prevention benefits with anti-HIV treatment, especially in developing countries, many programs have insufficient resources to provide coverage to those already in need. '[Antiretroviral treatment] appears to confer a significant prevention benefit across all CD4 ranges,' Donnell says, 'and this study quantifies that more accurately.'
From our Sponsors
Most Popular
“So much life to live”: Eric Nieves on thriving with HIV
September 03 2025 11:37 AM
Messenger RNA could be the key to an HIV vaccine — but government cuts pose a threat
August 20 2025 8:02 AM
It’s National PrEP Day! Learn the latest about HIV prevention
October 10 2025 9:00 AM
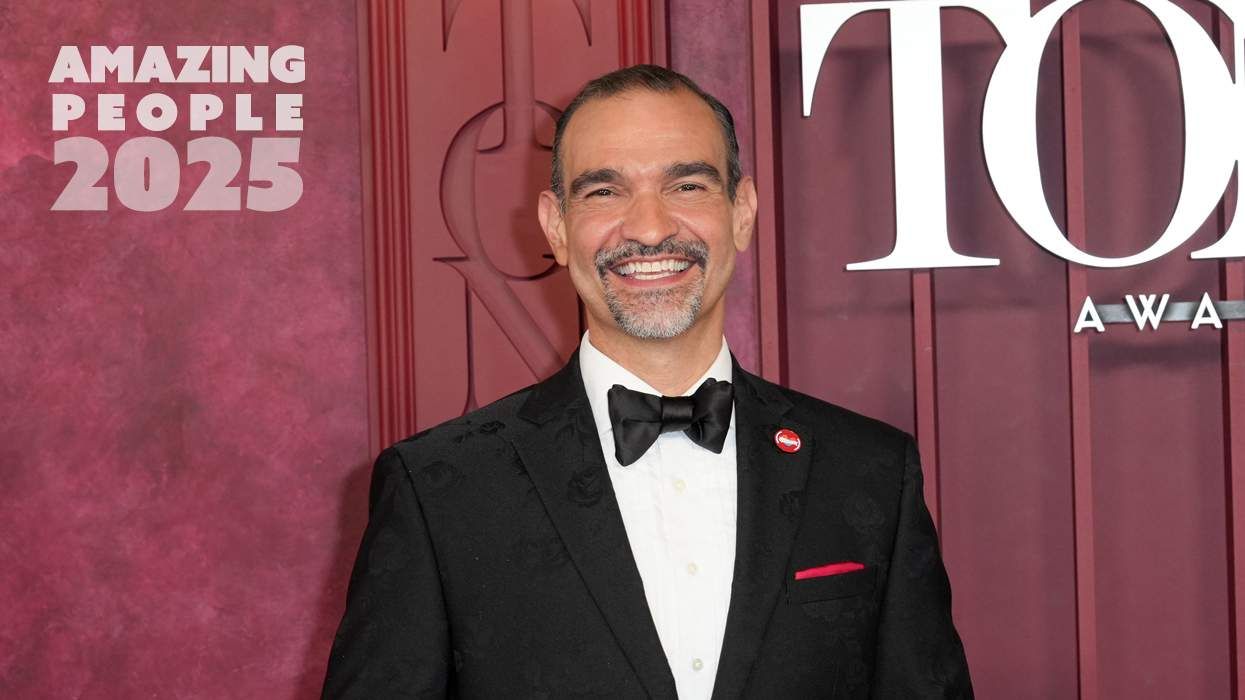
Amazing People of 2025: Javier Muñoz
October 17 2025 7:35 PM
The lab coat just got queer
August 21 2025 10:00 AM
The Talk: Owning your voice
August 25 2025 8:16 PM
“I am the steward of my ship”: John Gibson rewrites his HIV narrative
September 16 2025 2:56 PM
Plus: Featured Video
Latest Stories
HIV-positive men stage 'Kiss-In' protest at U.S.-Mexico border
December 01 2025 12:56 PM
What the AIDS crisis stole from Black gay men
December 01 2025 6:00 AM
The Talk: Beyond the exam room
August 13 2025 3:15 PM
The Talk: Navigating your treatment
August 01 2025 6:02 PM
The Talk: Starting the conversation
July 25 2025 4:47 PM
Thanks to U=U, HIV-positive people can live long, happy, healthy lives
July 25 2025 2:37 PM
How the Black AIDS Institute continues to fill in the gaps
July 25 2025 1:06 PM
“I felt like a butterfly”: Niko Flowers on reclaiming life with HIV
July 23 2025 12:22 PM
Dancer. Healer. Survivor. DéShaun Armbrister is all of the above
July 02 2025 8:23 PM
BREAKING: Supreme Court rules to save free access to preventive care, including PrEP
June 27 2025 10:32 AM
1985: the year the AIDS crisis finally broke through the silence
June 26 2025 11:24 AM
VIDEO: A man living with HIV discusses his journey to fatherhood
June 10 2025 4:58 PM
Trump admin guts $258 million in funding for HIV vaccine research
June 03 2025 3:47 PM
Grindr is reminding us why jockstraps are so sexy and iconic
May 02 2025 5:36 PM
HRC holds 'die-in' to protest Trump health care cuts
April 28 2025 2:11 PM
Two right-wing Supreme Court justices signal they may uphold access to PrEP and more
April 21 2025 4:10 PM