A change to New York State’s budget will take hundreds of millions of dollars away from clinics and hospitals treating low-income and underserved people, including those living with HIV — and health care providers and over 40 lawmakers are calling for a reversal.
The change involves the 340B Drug Pricing Program, a federal program under which certain providers serving the neediest people can obtain prescription drugs at deep discounts but bill insurance plans, including Medicaid, for the full price. The money representing the difference between the insurance payment and the discount price of the drugs can be kept by the provider to hire staff, expand services, and make other investments to improve care. This difference is known as the “spread.”
But under the budget adopted by the state legislature and signed into law by Gov. Andrew Cuomo, in order to save money on Medicaid, the 340B pharmacy benefit will be carved out from the Medicaid managed care program. The drugs will be switched to a fee-for-service arrangement, under which state will reimburse providers at cost, therefore wiping out the spread and expected to save the state $87 million, although opponents question this figure. New York has seen a reduction in tax revenues due to the economic fallout of the COVID-19 crisis, and state law requires a balanced budget.
But the state shouldn’t balance its budget on the backs of its neediest people, says Save New York’s Safety Net, a coalition of more than 40 health care providers and related organizations.
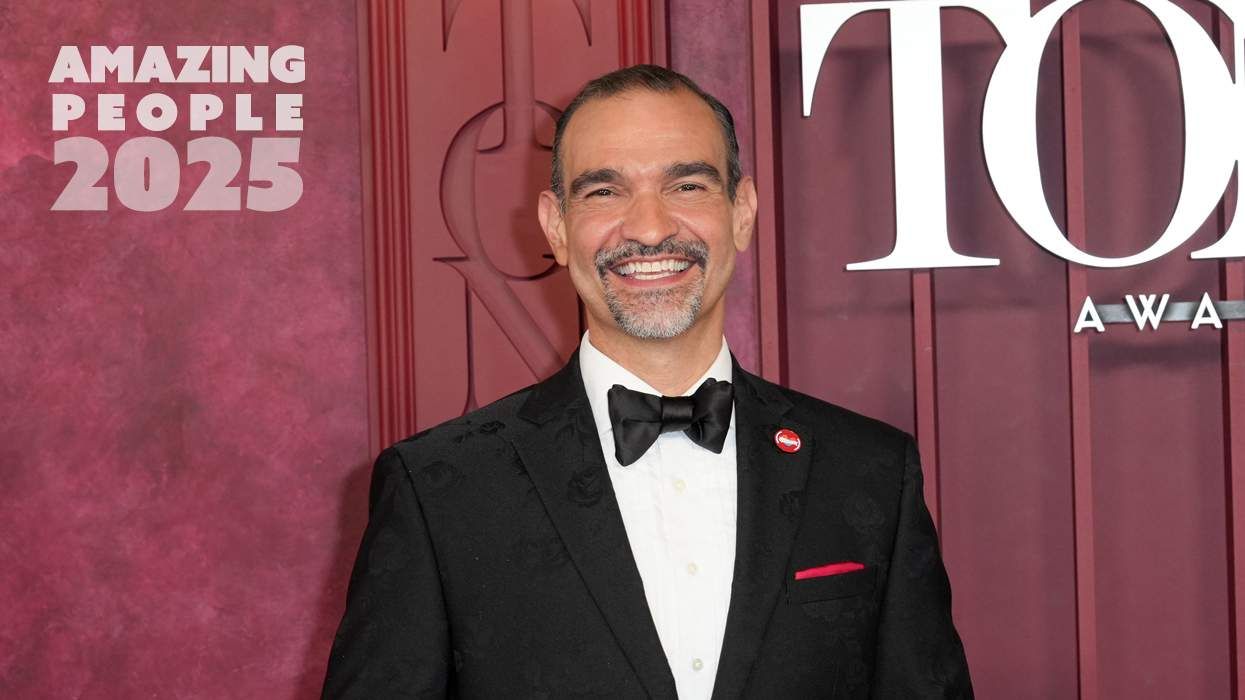
“HIV providers will lose hundreds of millions of dollars because of this policy change,” says Doug Wirth, CEO of Amida Care, an insurer that offers managed care services to New Yorkers living with HIV and those who are homeless or of transgender experience and therefore at heightened risk for the virus, and is part of the coalition. Those eligible for Medicaid in New York must choose a state-approved health plan to receive their care through, and that’s where groups like Amida Care come in, he explains.
“A broad coalition has come together to tell the state it’s bad policy and the savings contestable,” Wirth says. It’s also “shortsighted and counterproductive,” he says, threatening to undermine the success care providers had before the pandemic in enrolling and maintaining people in treatment, therefore helping them suppress their viral load.
The change is scheduled to go into effect April 1, coming at a time when HIV care providers are suffering because of COVID-19 and fewer clients have been coming in for testing and treatment, Wirth says. And when the COVID vaccine becomes available, these providers will need to step up their outreach to get people in to receive it, he adds.
The governor and the New York State Department of Health have the power to reverse the change, and the coalition is calling on them to do so and has suggested other places to find savings, such as in management of long-term care and reimbursements to third-party administrators. “Many, many health plans are opposing the carve-out and are willing to work with the state to achieve savings through other mechanisms,” Wirth says.
“The policy change is about balancing the state budget on the back of the HIV, Indigenous, and POC communities,” he adds.