The U.S. Conference on AIDS attracted more than 2,000 advocates, service providers, and people living with HIV or AIDS, and was centered around the theme “In It Till the End,” meant to reflect the momentous changes in our movement that, for the first time in more than 30 years, have made it possible to realistically envision an end to the epidemic.
But the Deep South is still in deep denial.
Kathy H. Kliebert, the interim secretary of Louisiana’s Department of Health and Hospitals and director of the state’s STI program, said the intersection of institutionalized racism, poverty, homophobia, health disparities, and lack of sex education explains why the southern states have the highest HIV and AIDS rates among African-Americans and gay and bisexual men.
“Where is the office of poverty?” Kliebert demanded, saying that now was the time for us to look at the number one cause of HIV in the southern region of the U.S.
The South accounts for only one third the U.S. population but almost half of all HIV infections. New Orleans is third in the nation for new HIV diagnoses, while Baton Rouge (just an hour north) ranks second, according to Kali Lindsey, the National Minority AIDS Council’s director of legislative and public affairs. Making matters worse, Louisiana is ranked sixth in the number of uninsured residents, but the state joined every other in the South in refusing to set up insurance marketplaces or take part in the Affordable Care Act’s Medicaid expansion.
According to the Centers for Disease Control and Prevention, the South is home to seven of the 10 states with the highest rates of AIDS diagnoses, eight of the 10 with the highest rates of new HIV infection, and six of the 10 with the highest cumulative rates of individuals living with HIV.
“Given the profile of the epidemic in the South and the region’s resistance to ACA implementation, it is especially critical that we highlight the unique challenges facing those working to combat HIV/AIDS here,” said Paul A. Kawata, executive director of the National Minority AIDS Council.
Here are just a few of the conference findings.
The ACA Changes Everything
Much of the work this year, said many presenters, will be in getting every eligible person enrolled in insurance under the ACA—commonly referred to as “Obamacare,” even by the president—now that open enrollment has begun. According to Health Resources and Services Administration, approximately 140,000 Americans living with HIV are eligible for expanded insurance coverage under the ACA. In addition to extending coverage to more people, the ACA requires HIV testing coverage, eliminates preexisting conditions exclusions and lifetime spending caps, and lets people stay on their parents’ insurance until age 26.
But It Still Needs Work
Leaving the decision to expand Medicaid up to each state was tantamount to “throwing HIV-positive poor people under the bus,” said Robert Greenwald, director of the Center for Health Law and Policy Innovation at Harvard Law School as well as the Treatment Access Expansion Project. Greenwald spoke to social workers, service providers, and activists about ensuring that all people with HIV are enrolled in an insurance program. In addition, he said, advocates must push for the Medicaid expansion that was originally planned—eight conservative Republican governors now have signed on to the expansion, and some others support alternative approaches, “such as the Arkansas premium assistance model; with safeguards in place it can work for low-income, uninsured people living with HIV.”
There’s an End in Sight—Sort Of
“For the first time since HIV emerged in 1981, we have a clear blueprint forward to end this epidemic,” said Lindsey. Hundreds of thousands of individuals living with HIV are newly eligible for insurance coverage—many for the first time in their lives, Lindsey said. “Meanwhile, biomedical advances like treatment as prevention and pre-exposure prophylaxis have demonstrated incredible efficacy in slowing HIV transmission and hold great promise in our efforts to reduce new infections.”
“When we join the Affordable Care Act with the science of ‘treatment as prevention’ and the National HIV/AIDS Strategy, we have a combination that can begin to end this epidemic,” added Kawata.
Getting Care in Rural Louisiana
The Southwest Louisiana AIDS Council announced the results of a two-year study, which looked at linkage to care and treatment adherence among people with HIV in the rural town of Lake Charles. Specifically, the study scrutinized the results of two of the AIDS Council’s programs, Facilitated Access to Coordinated Treatment and Treatment Adherence Program. Some of the findings:
- Over 95% of individuals enrolled in the two programs were linked to medical care over the two-year period.
- The percentage of people with an undetectable level of HIV in their blood increased to 56% in two years (a nearly 51% increase).
- Average CD4-cell counts increased from 322 to 460 at an average of 18 months post-enrollment. Similarly, there was a decrease in the average levels of HIV in the blood of participants at 18 months post-enrollment.
According to the Louisiana Department of Health and Hospitals, nearly half of all people living with HIV infection in Lake Charles were not in medical care in 2010.
“Linkage, retention, and adherence to care and treatment can be particularly challenging in rural areas, where there are fewer options for health care services and unique obstacles exist, such as the need to travel long distances to access these services,” said Russell Brewer, director of the HIV, STD, and Reproductive Health program at the Louisiana Public Health Institute. “Particularly in the southern United States, where the CDC estimates that 45% of all new AIDS diagnoses occur, it’s encouraging to see measurable outcomes from interventions that are getting people into care and providing the follow-up to help them over the long term.”
The Doctor Talk
A new online nationwide survey of more than 300 people living with HIV on antiretroviral therapy found them to be very engaged with their health care providers in the management of their HIV; nearly all (97%) said that they are proactive about managing their HIV condition, including drug treatment. However, the survey findings also showed that about three in four HIVers would like to spend more time discussing drug treatment with their doctors (74%) and the impact of HIV on their lives (71%), and only 39% indicated that they understand all the information shared by their doctors about the management of their drug treatment.
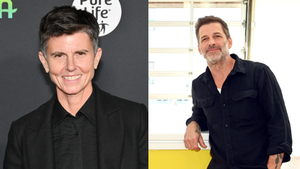
The survey, which examined the breadth and depth of communications between people living with HIV and their doctors, was meant to complement drug company Merck’s national HIV education campaign, I Design, which boasts as celebrity spokesmen photographer Duane Cramer (who was on the cover of HIV Plus in July) and Project Runway All-Stars winner Mondo Guerra (who was on the cover in 2012). I Design is intended to empower people living with HIV to have open and meaningful discussions with their doctors.
“As someone who has lived with HIV for close to 20 years, I know there are numerous topics to discuss during each visit to the doctor and can understand why many people may find it difficult to cover all of them,” said Cramer. “Preparing for discussions with my health care provider by prioritizing what I want to discuss about my medicines, my other health conditions, and relevant aspects of my life have been important factors to my HIV treatment plan over the years. This is what I encourage people to do as part of the I Design campaign.”
Respondents admitted they wanted to spend more time discussing certain matters with their doctors, including how their current HIV drug treatment regimen is working (selected by 40%), other HIV treatment options (30%), health conditions they have other than HIV (30%), side effects of their current HIV medications (28%), and taking their current HIV treatment as directed (13%). Respondents also indicated they would like to spend more time discussing the physical impact of HIV on their bodies (51%) and the impact of HIV on their sex lives (26%), day-to-day lives (25%), mental or emotional well-being (29%) and relationships with their loved ones or family (15%).
Gay, bisexual, and other men who have sex with men (MSM) represent approximately 2% of the U.S. population yet are the group most severely affected by HIV. In 2010, MSM accounted for 63% of all new HIV infections. That same year, MSM aged 13 to 24 accounted for 72% of new HIV infections among all people in that age group and 30% of new infections among all MSM. At the end of 2010, an estimated 489,121 (56% of the total) people with an HIV diagnosis in the United States were gay or bisexual men, or men who have sex with men but don’t identify themselves with those labels.

Stigma Project cofounders Chris Richey and Scott McPherson (HIV Plus’s former creative director) talked about these stats and the need for honest conversations about HIV in the gay community) as part of their new Gilead-sponsored Engage campaign. Several posters with messages about getting tested were released as part of the campaign, which is aimed at getting people with HIV into treatment, engaged in their own medical care, and having safe sex and conversations about it (because 47% of gay and bisexual men have reported that they don’t wear a condom every time they have sex). Richey, who is HIV-positive, talked about moving past the stigma of being poz and into a life where he could not simply continue living but actually thrive as an out HIV-positive, gay man.
Richey wasn’t the only person who talked about ending stigma; many presenters said that stigma itself was the number one thing that prevented people from getting tested. In a survey by Project Inform (see chart at right), 68% of HIV-positive people said that stigmatization was a major disadvantage to being poz.
Sisters Were Doing It for Themselves
Women were out in full force at the conference too, and some of the best presentations focused on trans women (56% of African-American trans women are HIV-positive) and how gender violence plays into HIV transmission and treatment. Meanwhile, an organization called Common Threads Marketplace, a microenterprise coalition of HIV-positive women, brought women from around the country to sell products in the exhibition hall. And the much-coveted USCA conference bag was made by former sex workers in Africa (who are paid a living wage and use recycled cloth). Participants got a beautiful reusable bag, but we also get to help women change their lives and the lives of their families.