One Out of 80 Million?
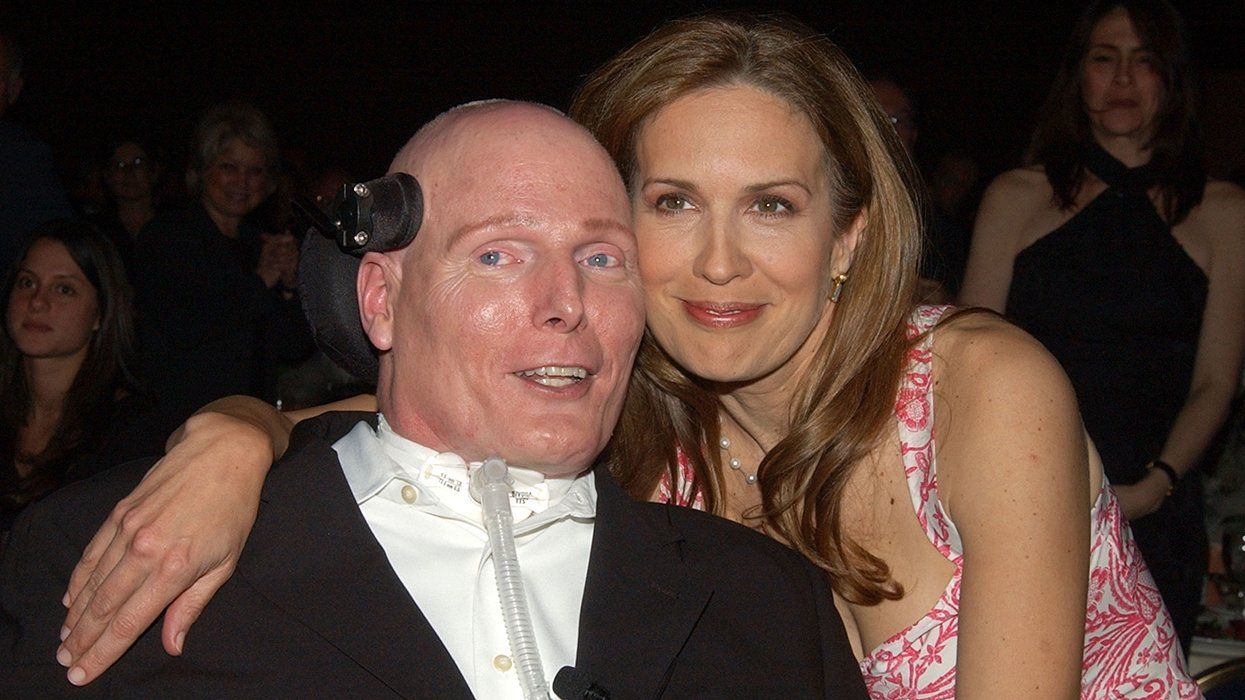
Timothy Brown may have been cured, but one out of 80 million isn’t great odds. That’s what Dr. David Margolis, head of the Collaboratory of AIDS Researchers for Eradication told the audience attending this summer’s HIV Cure Conference, which was hosted by CARE and the University of California, San Diego’s AntiViral Research Center. “A cure is feasible,” Margolis added. “But I want to manage expectations and convey the reality about this whole cure expedition and that is, it ain’t gonna happen fast.” Margolis sees the biggest hurdle to a cure being the way HIV can hide out of sight, becoming undetectable in the bloodstream, and yet rebounding later.
Waking Dormant HIV Essential to a Cure
Reservoirs of HIV are a major barrier to any cure because the current medications can’t find and treat the virus in those reservoirs, so many researchers are working on finding a way to activate and eliminate HIV reservoirs. Using synthesized compounds called “bryologs,” researchers have figured out how to wake up HIV in the lab and make it detectable “at least for a short time,” according to a study led by Jerry Zack of the David Geffen School of Medicine at the University of California, Los Angeles, and Paul Wender at Stanford University. But they still don’t know if they can clear the newly detectable virus and whether they have reached every cell that is infected.
Could The Immune System Turn Assassin?
Luring dormant HIV out of hidden reservoirs with bryologs or some other method is just the first step, say researchers at Johns Hopkins University School of Medicine. “Our results suggest that luring HIV out of hiding is winning only half the battle,” said senior investigator Robert Siliciano earlier this year. “We found that these pools of dormant virus carry mutations that render HIV invisible to the very immune cells capable of disarming it, so even when the virus comes out of hiding, it continues to evade immune detection.” In the lab, Siliciano’s team successfully trained immune sentinel cells known as “killer T cells” to spot and eliminate mutated strains of HIV. These T cells found and killed 61 percent of the HIV-infected cells.

How to Stop Mutants
That same John Hopkins study also discovered that patients who began antiretroviral therapy within a few weeks or months of infection harbored largely nonmutated HIV. Starting therapy early appeared to have halted the mutation process, freezing the virus more or less in its original state. By contrast, more than 98 percent of the virus in the latent reservoirs of late-treated patients was mutated. Treating — and eventually curing — HIV is much more difficult with mutated strains.

Is This HIV Kryptonite?
Canadian researchers have discovered another method for destroying once-dormant HIV after it has been awakened. They discovered a molecule, JP-III-48, that they dubbed the “can opener,” which tricks HIV into opening itself up to attack from antibodies that could kill the virus. The study, published in Proceedings of the National Academy of Sciences, builds on earlier findings in which cells infected with HIV-1 (the most common strain of HIV) were more easily eliminated when two HIV-specific proteins were deactivated. Because these two proteins protect HIV from attack, eliminating or deactivating them could leave the virus vulnerable and exposed. The JP-III-48 molecule mimics the CD4 protein, so HIV opens itself up, expecting the CD4 protein to enter. In doing so, it becomes vulnerable to immune system attacks. Then antibodies that are naturally present in people with HIV can target those infected cells. The Canadian researchers see the molecule playing a part in a “shock and kill” approach to eliminating HIV reservoirs. “We have to reactivate HIV reservoirs to force the virus out of its hiding place,” said Dr. Andrés Finzi, the study’s author. “Then kill the infected cells with this molecule and the already present antibodies.”

Already Safe for Humans
At this year’s Cure Conference, scientists reported that HIV is actually “a disease of the lymphoid tissue.” In other words, only 1 percent of a person’s T cells are located in the bloodstream, while 98 percent of CD4 T cells reside in lymphoid tissues, where HIV behaves differently than in the blood. Dr. Warner Greene has discovered that T cells in lymphoid tissue launch an attack not on the virus itself but on pieces of human DNA that are discarded as HIV replicates. In doing so, the T cells release inflammation, which draws more T cells to the spot, where they also die. The cells essentially commit suicide in a vain attempt to protect the larger host. Ending that deadly cycle, Greene believes, could reduce HIV’s impact on a person’s health, basically making their viral load irrelevant to their condition. His team has already discovered what will stop this cycle: caspase-1 inhibitors, caspases being substances that play an important role in cell death. Already in clinical trials for other applications, a caspase-1 inhibitor called VX -765 has proved safe in humans, but it would need Food and Drug Administration approval before it could be prescribed to treat people with HIV.
Sugar and Spice, Anything But Nice
A new study indicated that HIV has a voracious sweet tooth, which can be used against it. When the virus enters an activated immune cell, it needs energy to replicate, which it gets from sugar and other nutrients. Cut off the supply of sugar, the theory goes, and HIV can’t replicate in the cell. Researchers at Northwestern Medicine and Vanderbilt University say they’ve found a way to cut off the sugar pipeline and starve the virus. This novel approach, which could also work on cancer (another disease with a powerful sweet tooth), has several benefits, including the reduction in organ damage in people with HIV. The virus causes an abnormal proliferation of immune cells, which can lead to inflammation and damage to organs over time, even in patients who are on antiretroviral treatment. “This discovery opens new avenues for further research to solve today’s persisting problems in treating HIV infection: avoiding virus resistance to medicines, decreasing the inflammation that leads to premature aging, and maybe even one day being able to cure HIV infection,” said Richard D’Aquila, director of Northwestern’s HIV Translational Research Center.

Kick and Kill, But Not for a Decade
Research published in Clinical Infectious Diseases in May introduced what an international team has called the “kick and kill” strategy — a different way of saying “shock and kill” — for eliminating HIV. Researchers from England’s University of Oxford, the University of North Carolina at Chapel Hill, and the University College London Hospitals NHS Foundation Trust (a collection of eight hospitals that are part of England’s National Health Service) believe it’s possible to use an HIV vaccine as a stepping-stone to an HIV cure. Their strategy would first use a vaccine to stimulate the immune system; then the HIV lying dormant in hidden reservoirs would be reawakened with a chemical “kick.” Although promising, this group’s research on “kick and kill” revolves around the experience of a single subject, an “elite controller” — someone whose immune system can control HIV for an extended period without treatment. The immune system of the study’s subject was able to subdue HIV as well as antiretroviral medication would. Scientists hope to develop a vaccine from elite controllers. Study coauthor Dr. Ravi Gupta cautions, “Drugs to stimulate reactivation of dormant HIV are still imperfect, and we do not know if they would be able to flush out all of the HIV from the body. Likewise, it remains to be seen whether a vaccine could enable a normal HIV patient’s immune system to kill HIV with the full strength of an elite controller. Our study is a proof of principle and the results are promising, but it is unlikely to lead to a cure for at least a decade.”
Do Elite Controllers Hold the Key?
The aforementioned study isn’t the only one looking at the possibility that elite controllers could hold the key to an HIV vaccine or cure. For example, University of California, Davis, researchers are studying 61-year-old Californian Loreen Willenberg, who has been HIV-positive for more than two decades, has never taken HIV medications, and yet remains symptom-free. In fewer than 1 percent of those who are HIV-positive, the immune system seems capable of controlling the virus and preventing it from damaging cells, Dr. Richard Pollard of UC Davis told a Sacramento TV station. There are reportedly only 500 of these elite controllers in the world. “Their body has such an effective way of reacting to the virus that it’s hard to even detect that they’re virus-positive,” said Pollard. In most cases, once HIV has entered a person’s bloodstream it attacks the white blood cells known as CD4 T cells. HIV kills T cells and replicates itself, while also fighting off immune system responses, including those from healthy CD8 cells that usually combat viral infections. In people like Willenberg, however, CD8 cells remain strong and regulate infected CD4 cells, which keeps HIV from replicating. Finding a way to harness what makes her and other elite controllers special may well help researchers develop a vaccine or a cure.

Tinkering With Genes Could Lead to a One-Shot Cure
Genetic variations that provide natural resistance to HIV (like the ones that elite controllers have) are central to some researchers’ efforts to develop a cure. One of the doctors responsible for curing Timothy Ray Brown, the so-called Berlin patient, is focusing on gene therapy based on a genetic variation and believes he’s closing in on a one-shot HIV cure. “I believe it’s possible to develop a mass-market single-shot treatment for HIV,” Dr. Gero Hütter told U.K. newspaper The Guardian. “If we can overcome a few problems, our approach is closer to a complete cure than anything in the last 30 years.” Brown was cured with a bone marrow transplant from a donor who had a natural immunity to HIV. About 1 percent of the population has that donor’s rare gene mutation, which prevents HIV from binding to white blood cells by disabling its typical receptor target, CCR5. So far all efforts to replicate the Brown results have failed — aside from the Barcelona patient who was reportedly cured for several years before dying of cancer — but Hütter still believes that CCR5 holds the key.
…Or a Vaccine
Dr. Michael Farzan also thinks CCR5 is the answer. The Harvard University professor is famous for discovering the benefits of the CCR5 mutation 16 years ago. He recently told The Guardian he’s close to developing an HIV vaccine based on this same genetic immunity. Farzan said his potential vaccine would bind to HIV and prevent it from invading white blood cells. “This isn’t a cure,” Farzan was quick to explain. “A cure would remove all evidence of the virus from the body, and we don’t have that ability.” Still, Farzan hasn’t written off those who are already poz; in fact, he said his vaccine could provide people with HIV what he calls a “biologic remission, which means they can live without drugs.” While some of the other efforts to develop an HIV vaccine focus on stimulating (and sometimes enhancing) the body’s natural immune response, Farzan’s approach is to block cell receptors that the virus can attach to, thus preventing it from latching on and replicating. Farzan acknowledged that some strains of HIV are capable of simply finding other receptors to attach to, but he said, “Those strains of HIV are extremely rare, so if it moves away from the common receptors, this will come with what we call a fitness cost for the virus. Because there are fewer strains, they are less replicative and transmissible.”
…Or Even Just Resistance to Infection
University of Minnesota scientist Reuben Harris is studying serodiscordant couples who’ve retained their mixed HIV status without medication, despite many opportunities for the virus to be transmitted to the negative partner. Harris believes the answer lies with a family of genes called APOBEC3, which produce antiretroviral enzymes. Harris discovered that a specific variation to the gene APOBEC3H produces stronger and more stable antiretroviral enzymes, which appear to impede the replication of HIV. Those with the gene variation aren’t totally immune, but they are less likely to contract the virus. Harris told The Guardian that gene therapy based on the APOBEC3H variant could help make certain populations less susceptible to HIV. In this case, studies show that few Caucasians naturally have the optimal version of the gene, so they could benefit from this therapy. “These enzymes are really powerful virus inhibitors,” Harris said. “And it may be possible to suppress infection completely by unleashing them to a greater extent.… There are probably lots of different ways that people can resist infection. I guess it’s a perfect example of why we don’t want homogeneity in the human race. If we were all the same, then it would be too easy for a super-virus to sweep through and wipe us all out.”

Monkey See, Monkey Do — Er, Don’t
We reported last April on a monkey vaccine that blocked simian immunodeficiency virus (SIV, HIV’s primate relative) and quickly suppressed the viral loads of monkeys. Researchers hoped that the monkey vaccine could be the first step to creating a human vaccine for HIV, but findings of a new study show the monkey vaccine to be less effective than previously thought, calling into question a central assumption in how a human vaccine might work. Previously, researchers had thought that an HIV vaccine could protect people from getting the virus by stimulating moderate levels of antibodies to neutralize it. But these scientists found that SIV still managed to infect monkeys that had been vaccinated, even though potent neutralizing antibodies were found in the monkeys’ blood. The scientists had expected that any virus that could infect a vaccinated monkey must have mutated to develop a resistance to the vaccine. But that’s not what happened. The study, published August 10 in Proceedings of the National Academy of Sciences, revealed that the vaccinated monkeys were exposed only to the same strain they’d been vaccinated against. The researchers said the vaccine protected some monkeys from SIV infection, but it was not foolproof and may not remain effective through multiple exposures. More research is needed to fully explain the failure, but in the meantime scientists can’t proceed to human trials as quickly as they’d hoped.

Don’t Let Jenny McCarthy Hear This
Three new studies demonstrate how a series of vaccinations could “prime” the immune system in anticipation of attacking HIV. Each vaccination would build on the other, as many childhood vaccines do, preparing the immune system so it can make antibodies that neutralize an entire spectrum of HIV strains. If HIV later enters the body, the immune system is able to fight off the infection. Scientists at the Scripps Research Institute set out to mimic the antibodies produced by elite controllers and use them to protect HIV-negative individuals from contracting the disease. The first step is to stimulate the immune system to make more of a subtype of B cells that can produce these broadly neutralizing antibodies. They created two engineered molecules that trigger the production of increasingly mature antibodies (one was, according to Science, shown to be an effective HIV vaccine in rabbits). HIV is covered in proteins that confuse the immune system, which attacks them instead of noticing the more vulnerable regions. By mimicking the receptors that HIV usually attaches to, the molecules trick the virus into attaching to them, thus rendering it incapable of replicating.

Heads or Tails?
A promising new treatment could prevent HIV without the need for a vaccine, and so far in monkey trials it has appeared to be effective even against the most virulent and treatment-resistant strains of HIV. Published in Nature, the findings indicate that a particular compound, a protein dubbed eCD4-Ig, which resembles normal antibodies but has both a head and a tail, can block two receptors at once. If HIV can’t attach to either receptor, it cannot infect the cell and is rendered harmless. So far the research has been very limited and exclusively on monkeys, but four monkeys given the compound remained HIV-free despite repeated attempts to infect them over a 12-month period.

The Real Cock Block
Researchers say a newly discovered tweezer-shaped molecule delivers a two-pronged attack on HIV in semen and may also be effective against hepatitis C, herpes, the flu, and Ebola. The molecule, CLR01, has shown positive results in laboratory tests, leading an international team of scientists at the University of Pennsylvania and Germany’s Ulm University to suggest the molecule could effectively prevent HIV transmission as a vaginal or anal gel. “We think that CLR01 could be more effective than other microbicides that are in development because of its dual action, its safety in terms of side effects and its potential broad application,” noted James Shorter, coauthor of the study, published in the journal eLife.
Less Is More?
Studies in France and the United Kingdom have shown that Truvada, the only drug currently approved for the prevention of HIV, continues to work even when the dose is lowered. While it’s successful at preventing HIV transmission nearly 96 percent of the time when taken daily, tests showed that when taken less frequently but at particular key times, Truvada as pre-exposure prophylaxis, or PrEP, still lowered HIV risk by 86 percent. Patients are urged not to increase their risks by breaking with their daily regimen, though. The Food and Drug Administration has only approved a daily dosage for PrEP, and there’s more testing to be done to see if these results can be repeated. “We don’t want people to potentially put their lives at risk from taking the wrong kind of PrEP regimen,” said Jennifer Horvath, deputy director of news media at the Centers for Disease Control and Prevention.

A New Kind of Monthly
A new implanted device could revolutionize HIV treatment by making it so people with HIV don’t have to take another pill, making it so more people would adhere to treatment. The matchstick-size device is designed to be implanted under the skin, where it can automatically deliver carefully measured doses of antiretroviral drugs. The device has undergone animal trials, and the findings, published in Antimicrobial Agents and Chemotherapy, showed it successfully delivered a controlled, sustained release of antiretroviral drugs for up to 40 days. Adherence has been shown in clinical trials to be one of the most significant factors in determining successful HIV outcomes, and it is widely viewed as one of the most critical elements in the fight against HIV. Some patients struggle with adherence, especially if they are prescribed numerous drugs — whether to enhance drug effectiveness, provide cheaper treatment options, fight multiple HIV strains, or prevent the virus from becoming drug-resistant. “This novel device will revolutionize how we treat or prevent HIV/AIDS,” said Dr. Marc Baum of California’s Oak Crest Institute of Science, which developed the device. “It delivers powerful HIV-stopping drugs and eliminates one of the key obstacles in HIV/AIDS prevention — adherence to proper dosing regimens.” Moving forward with plans for human trials, the institute is also working to extend the effectiveness of the implant: Researchers hope eventually to have one that can remain effective for an entire year.
The Strain(s)
A study published in PLOS Medicine suggests that only a handful of mutations are responsible for the majority of drug-resistant HIV strains. Researchers at Stanford University School of Medicine focused specifically on medications used to treat infections in resource-limited settings (particularly nonnucleoside reverse transcriptase inhibitors) and discovered that a limited number of mutations are behind most cases of transmitted drug-resistant HIV around the world. Like other viruses, HIV has the ability to mutate in response to environmental factors, including the presence of antiviral drugs, and those mutations can then be transmitted from one person to another. The Stanford study is the largest of its kind, examining 50,000 patients in 111 countries. The fact that a small group of mutations accounted for a majority of the cases of transmission-related drug-resistance suggests that the number of these drug-resistant strains has not increased dramatically, as was previously feared.

Who Needs Aquaman?
A marine sponge may hold the key to reducing HIV hiding in reservoirs in the body, say scientists at the Florida campus of the Scripps Research Institute in a study published in the journal mBio. Unlike traditional antiretrovirals, the natural compound Cortistatin A reduces residual levels of HIV from these infected dormant cells, establishing a near-permanent state of latency and greatly diminishing the virus’s capacity for reactivation, they say. Cortistatin A was isolated from a marine sponge, Corticium simplex, in 2006, and in 2008, Scripps chemist Phil Baran was the first scientist in the world to synthesize the compound. HIV-positive people given the compound saw viral reactivation a reduced by an average of 92.3 percent. “Our results highlight an alternative approach to current anti-HIV strategies,” said Susana Valente, the Scripps associate professor who led the study. “Prior treatment with Cortistatin A significantly inhibits and delays viral rebound in the absence of any drug. Our results suggest current antiretroviral regimens could be supplemented with a Tat inhibitor [Tat is a protein that helps the virus reproduce] such as Cortistatin A to achieve a functional HIV-1 cure, reducing levels of the virus, and preventing reactivation from latent reservoirs.”
Stick to It, Mister
Early HIV treatment has already been shown to provide long-term advantages, but a new French study reports that any immune recovery benefits gained by starting antiretroviral medications early may be lost if treatment is later interrupted. The findings, published in the journal AIDS, suggest that only combining early treatment with continuous lifetime adherence gives patients the best hope of reaching a near-normal ratio of CD4 to CD8 cells, which combine to do the work of fighting the virus. “While most people prescribed [antiretroviral therapy] eventually develop a near-normal CD4 count, only those who started treatment soon after infection, who have continued it ever since and remained undetectable, stand a more-than-even chance of achieving an immune system where the balance of T-lymphocytes resembles that of a person without HIV in terms of their CD4:CD8 ratio,” reported AIDSMap.

Make it Rain
More money was funneled into HIV research in 2015 than ever before, with amfAR, the Foundation for AIDS Research, creating a $100 million investment strategy in support of its Countdown to a Cure for AIDS initiative, launched last year with the goal of coming up with a functional cure by 2020. The establishment of the amfAR Institute for HIV Cure Research within a major academic research institution with a grant of $20 million is the centerpiece of the investment strategy, which Kevin Robert Frost, amfAR’s chief executive officer, called “the greatest expansion of amfAR’s grantmaking in the 30-year history of the foundation.” The institute, he said, brings cure researchers under one roof to “facilitate the rapid sharing of knowledge and ideas and create the kind of synergy needed to accelerate the search for a cure.”
Meanwhile, the Centers for Disease Control and Prevention announced it is investing $216 million in new funding to strengthen HIV prevention efforts throughout the country. ViiV Healthcare put $3 million into a program called Positive Action, aimed at lowering HIV’s impact on gay and bi men and transgender people around the world by tackling discrimination and stigma based on sexual orientation, gender identity, and HIV status. Several municipalities put big money into PrEP education and outreach (San Francisco, New York) in attempts to connect residents to funding sources like Medicare, while Washington State began paying for PrEP in full for residents who are aren’t insured and covering insurance co-pays for those who are.
And back on the cure front, pharma giant GlaxoSmithKline, maker of HIV meds such as Tivicay, dedicated $20 million to establish a research center with the University of North Carolina at Chapel Hill dedicated solely to finding a cure for HIV. One of its primary focuses will be on the “shock and kill” approach. “The ‘shock and kill’ approach has shown significant promise in early translational research on humans and has been the focus of research for the last several years,” said Dr. David Margolis, the professor of medicine at UNC-Chapel Hill who also heads CARE, at that San Diego HIV Cure conference. He is one of the first researchers to come up with the “shock and kill” proposal: to reactivate the dormant virus and make it visible to be attacked by the body’s immune system. In 2012, Margolis published promising results from a clinical trial that used the drug vorinostat (originally developed for blood cancers of T cells) to shock the HIV awake.