Is a Texas health insurance carrier discriminating against HIV patients? That’s what the HIV+Hepatitis Policy Institute is alleging in a recent complaint filed by the advocacy group.
Houston-based Community Health Choice Texas is offering “substandard HIV drug coverage by not covering recommended drugs for HIV treatment,” according to HIV+Hep. The group adds that the insurance company is placing most of the HIV drugs that it does cover on the highest and mostly payment tier, pushing more of the cost on patients.
The complaint was filed with the Center for Consumer Information and Insurance Oversight — a government agency that helps implement reforms to the Affordable Care Act — and includes accusations that Community Health Choice Texas is acting in a deceptive manner by listing over 100 HIV drugs it covers, even though over half of those are actually not covered. Of those HIV drugs that are covered by Community Health Choice Texas, many are formulations of the same generic drug, while some were actually discontinued years ago for severe side effects or lack of efficacy, according to HIV+Hep.
Community Health Choice Texas currently does not cover many single tablet regimens, forcing patients to take numerous drugs to keep their HIV in check, something common in the 2000s and 2010s. The federal government has stated forcing patients to unnecessarily take multi-drug regiments is discriminatory, according to HIV+Hep.
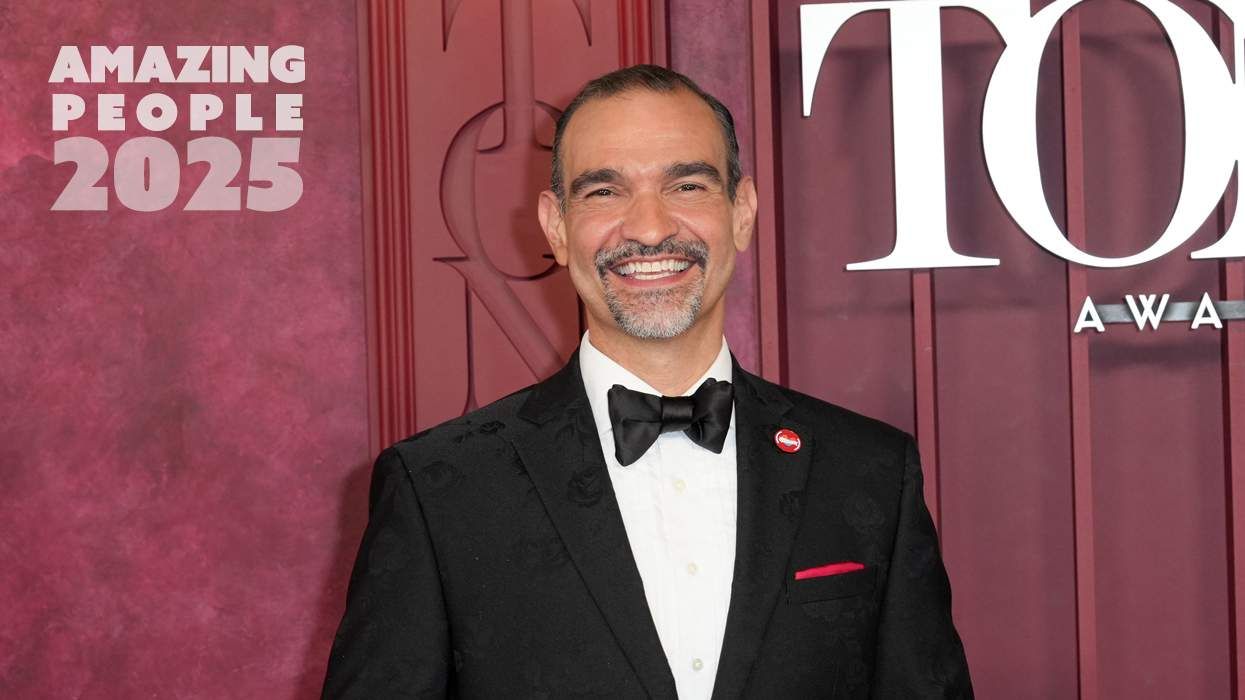
“We have seen a long-standing practice of some insurers that continue to discriminate against people with HIV in the way they design their benefits. We also continue to hear of people who are using PrEP to prevent HIV being illegally charged by their insurers for this zero cost-sharing preventive service,” Carl Schmid, executive director of the HIV+Hepatitis Policy Institute, said in a statement. “Without strict oversight and enforcement by federal and state regulators, insurers will continue to try to get away with as much as they can. That needs to stop.”
HIV+Hep wants the government to step in immediately and ensure that Community Health Choice Texas revise its coverage formularies for 2024. Schmid and his organization point out that making HIV meds more expensive and harder to obtain endangers public health as it discourages adherence and limits the reach of U=U, or undetectable equals untransmittable.
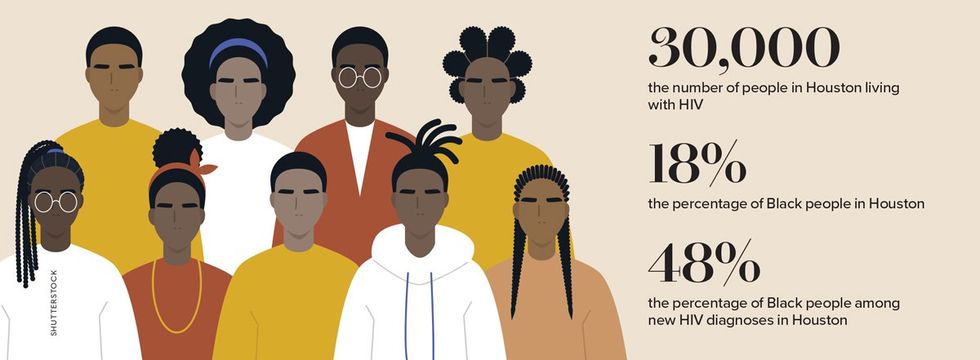
“Houston is one of the Phase I communities targeted by the federal government to end HIV due to the high prevalence of HIV in the county, which primarily impacts Black people,” notes HIV+Hep in a press release.
 Shutterstock
Shutterstock
From Your Site Articles
Related Articles Around the Web

 Shutterstock
Shutterstock