Treatment GuideJust DiagnosedSex & DatingAfrican AmericanStigmaAsk the HIV DocPrEP En EspañolNewsVoicesPrint IssueVideoOut 100
CONTACTCAREER OPPORTUNITIESADVERTISE WITH USPRIVACY POLICYPRIVACY PREFERENCESTERMS OF USELEGAL NOTICE
© 2026 Pride Publishing Inc.
All Rights reserved
All Rights reserved
By continuing to use our site, you agree to our Privacy Policy and Terms of Use.
If you think condoms are the only option when it comes to your safe-sex toolbox, think again. Today, there is quite the arsenal of prevention methods at your disposal when it comes to protecting yourself and your sexual partner. But just like with any tool in the toolbox, it is vital that you know how to use it so you don’t end up hurting yourself or someone else. So let's open our sexual safety kits and get to work.
1. The Condom
Let’s start with the basics. Condoms are still an excellent way to practice safe sex. When worn correctly, a condom is extremely effective in preventing the transmission of HIV. For gay men, the consistent use of condoms is 76 percent effective in preventing new HIV infections during anal sex. When used correctly and without error, a condom is up to 99 percent effective in preventing HIV transmission. Condoms are also effective in preventing most other STIs, but are not as effective in preventing the transmission of herpes, Hepatitis B or HPV.
The great thing about condoms is that they are cheap, easy to buy and use, and do not require a prescription.
2. Pre-exposure Prophylaxis, a.k.a. PrEP
As the latest one of the tools to be added to the toolbox, PrEP has experienced its fair share of controversy since the FDA approved Truvada for PrEP in 2012. Although some may disagree on when PrEP should be used and when it shouldn’t, the facts remain the same. When taken daily, PrEP prevents the transmission of HIV by up to 96 percent. To use PrEP, a person must meet with their healthcare worker to conduct blood work to determine that they are HIV-negative, and he or she must return every three to four months for blood screening. Although most side effects are temporary, about one in every 200 people will experience a change in kidney function, so PrEP users will need to keep up with their lab work to ensure that their kidneys are functioning properly. Most insurance providers do cover PrEP and there are several assistance programs for people who need additional help. People who use PrEP can stop using the prevention pill if they determine they do not need it anymore.
3. Treatment as Prevention a.k.a. TasP
You may have heard about when an HIV-positive man or woman achieves an undetectable HIV viral load from consistent adherence to their HIV medication. This excellent achievement in HIV care is also a form of prevention known as Treatment as Prevention, or TasP. When a person who is living with HIV has an undetectable viral load, they are 96 percent less likely to transmit HIV. But just like someone who says they are HIV-negative, you cannot be sure that someone is undetectable unless you know that they are compliant with their HIV medication and stay up-to-date with their regular lab work. Although TasP is an excellent reason to not be afraid of pursuing sexual and romantic relationships with people who are living with HIV, you should still take measures to protect yourself until you know that your sexual partner is, in fact, undetectable.
4. Post Exposure Prophylaxis, a.k.a. PEP
If PrEP is considered the HIV control pill, then PEP would be the HIV morning after pill. If someone believes that they have had unprotected sexual contact with someone who is HIV-positive, they can take PEP as a way to reduce their chances of becoming HIV-positive. The drug keeps HIV from making copies of itself and spreading throughout your body. A person must take PEP within 72 hours of contact and will need to continue the 2-3 antiretroviral combination therapy for 28 days. PEP can cause minor side effects such as nausea and loose stools and is not always effective in preventing a person from becoming infected with the virus. So as far as prevention methods go, PEP should be considered an emergency backup option instead of a daily approach to safe sex.
5. Strategic Positioning, a.k.a. Sero-Positioning
When it comes to HIV, it is the receptive partner, or the bottom, who is most at-risk for contracting HIV. So strategic positioning, or sero-positioning, is when a person chooses a different sexual position or practice depending on the HIV status of their partner. For instance, an HIV-negative man would choose to be the top and an HIV-positive man — or a man whose HIV status is unknown — would choose to be the bottom. Although strategic positioning is commonly practiced, few studies have assessed just how effective this prevention method is. HIV Plus previously reported on a 2012 study that found sero-positioning to be 75 percent effective in reducing infections. It is important to note that while the chance of the insertive partner becoming infected with HIV is markedly lower, it is not zero. In other words, tops can still becoming infected with HIV from their receptive partner, but the likelihood is lower.
6. Sero-Sorting
Sero-sorting is the practice of choosing a person’s sexual partner based on their HIV status as a way to prevent the transmission of HIV. Although this form of prevention can be effective when dealing with two HIV-positive people who are concerned with spreading the virus, it is not as effective in preventing HIV-negative people from becoming infected. More than half of all young gay men living with HIV are unaware of their status, making the sero-sorting strategy a difficult one to adhere to for casual sex. Unless you can be certain that your sexual partner has not engaged in any risky sexual activity since his or her last HIV test, you cannot be certain of his or her HIV status. HIV Plus previously reported on a study that found this option had only a 51 percent reduction in HIV infections.
7. Honesty
Oh yes! We saved the best method for last. Out of all of the tools in the toolbox, honesty is the most effective when it comes to preventing HIV. Whether it is being honest with yourself or with your sexual partners, telling the truth about your HIV status, your last HIV test and your desire to stay HIV-negative, or keep your partner from contracting the virus, can have up to a 100 percent efficacy ratio when used correctly. It doesn’t matter whether you are a top or a bottom, HIV-positive or HIV-negative, using honesty will allow you to combine other methods of prevention to ensure your safety without taking away from your ability to have a good time in the sack.
From Your Site Articles
From our Sponsors
Most Popular
“So much life to live”: Eric Nieves on thriving with HIV
September 03 2025 11:37 AM
The Talk: Beyond the exam room
August 13 2025 3:15 PM
Messenger RNA could be the key to an HIV vaccine — but government cuts pose a threat
August 20 2025 8:02 AM
It’s National PrEP Day! Learn the latest about HIV prevention
October 10 2025 9:00 AM
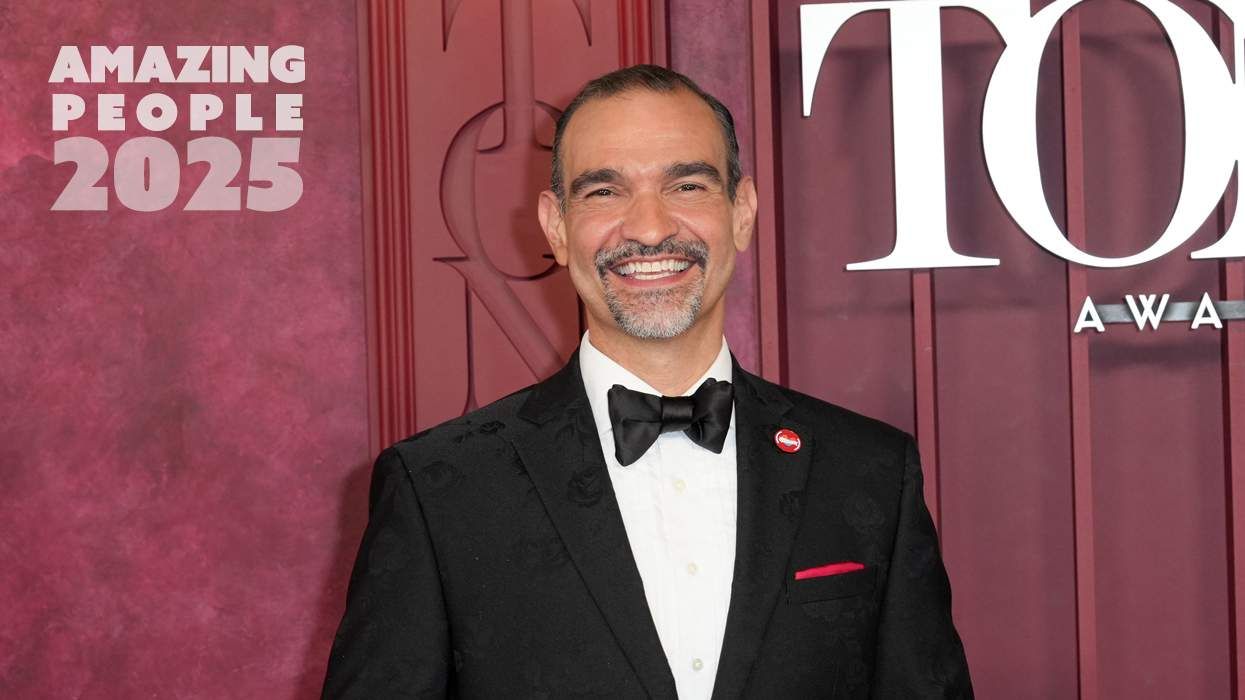
Amazing People of 2025: Javier Muñoz
October 17 2025 7:35 PM
The lab coat just got queer
August 21 2025 10:00 AM
The Talk: Owning your voice
August 25 2025 8:16 PM
The Talk: Navigating your treatment
August 01 2025 6:02 PM
“I am the steward of my ship”: John Gibson rewrites his HIV narrative
September 16 2025 2:56 PM
Plus: Featured Video
Latest Stories
HIV-positive men stage 'Kiss-In' protest at U.S.-Mexico border
December 01 2025 12:56 PM
What the AIDS crisis stole from Black gay men
December 01 2025 6:00 AM
The Talk: Starting the conversation
July 25 2025 4:47 PM
Thanks to U=U, HIV-positive people can live long, happy, healthy lives
July 25 2025 2:37 PM
How the Black AIDS Institute continues to fill in the gaps
July 25 2025 1:06 PM
“I felt like a butterfly”: Niko Flowers on reclaiming life with HIV
July 23 2025 12:22 PM
Dancer. Healer. Survivor. DéShaun Armbrister is all of the above
July 02 2025 8:23 PM
BREAKING: Supreme Court rules to save free access to preventive care, including PrEP
June 27 2025 10:32 AM
1985: the year the AIDS crisis finally broke through the silence
June 26 2025 11:24 AM
VIDEO: A man living with HIV discusses his journey to fatherhood
June 10 2025 4:58 PM
Trump admin guts $258 million in funding for HIV vaccine research
June 03 2025 3:47 PM
Grindr is reminding us why jockstraps are so sexy and iconic
May 02 2025 5:36 PM
HRC holds 'die-in' to protest Trump health care cuts
April 28 2025 2:11 PM
Two right-wing Supreme Court justices signal they may uphold access to PrEP and more
April 21 2025 4:10 PM
500,000 Children at Risk: PEPFAR Funding Crisis
April 08 2025 3:51 PM
Broadway's best raise over $1 million for LGBTQ+ and HIV causes
April 03 2025 7:15 PM