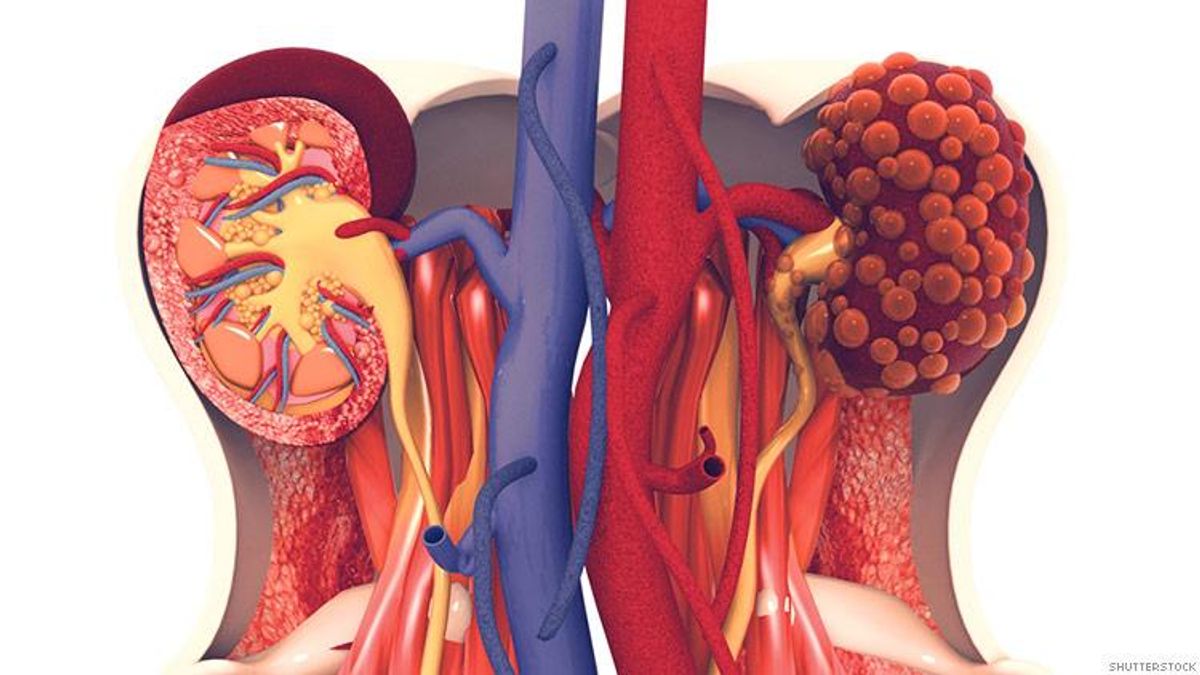
After her kidneys failed from the same illness that took the lives of her mother and brother, Anne Rupp went on dialysis in May 2016, spending three hours a day, three times a week undergoing the blood-cleaning procedure. She hated it
Rupp, who had polycystic kidney disease, joined more than 95,000 other Americans on kidney transplant lists. She knew the wait could stretch out for years.
But an experimental — and controversial — source of donated organs provided a far quicker resolution: Expensive medicines to treat hepatitis C have made it possible to use organs donated by victims of opioid overdoses who were infected with the once-deadly virus.
Six months after agreeing to be in a study in which patients in need of a kidney transplant would accept infected donor organs, Rupp got a 7:30 a.m. call at her home in York, Pa. “We have a kidney for you!”
The number of people donating organs after dying from drug overdoses has risen more than 200 percent since 2012, data from the United Network for Organ Sharing (UNOS) show — more than 13 percent of donors overall. About 30 percent of the 1,382 overdose-death donors in 2017, however, tested positive for hepatitis C.
In the past, organs exposed to hep C were typically discarded or given only to patients who already had the illness. Using them in patients who don’t have the virus could shorten the transplant wait time for hundreds of patients each year.
“This is super exciting because five years ago 100 percent of [the donated] hep C hearts were being buried and now some are being used,” said Dr. Peter Reese, an associate professor at University of Pennsylvania. “The world has changed.”
But patients who receive such organs would almost certainly need simultaneous treatment with drugs to treat hepatitis C, generally a six- to 12-week course of drugs that costs tens of thousands of dollars. And it’s unknown whether long-term use of the drugs is safe and effective in this population.
“‘We haven’t done this before,’” Rupp, 76, remembers her doctor at Johns Hopkins Hospital in Baltimore telling her when he offered her the option. But, he explained, the new antiviral medications nearly always cure hepatitis C.
While some hep C patients have no symptoms, over time, the untreated virus can cause chronic liver disease and lead to liver failure.
The Hopkins study — and several others nationally — are opening up new medical possibilities, while exposing patients to potential costs.
Since the procedure is considered experimental, many health plans don’t have a specific coverage policy on the expensive antiviral drugs that go hand in hand with it.
Insurers that responded to questions for this story generally said they take each request on a case-by-case basis, and cover the drugs if they deem them medically necessary.
Researchers and ethics experts say coverage must be clarified before the new procedure becomes more widely available.
“How can you intentionally infect someone if not 100 percent sure their third-party payer will pay for [treatment] it?” said Dr. Christine Durand, an assistant professor of medicine at Johns Hopkins University School of Medicine.
At Hopkins, patients start the antiviral drugs just before being wheeled into the operating room. Other programs wait until the patient tests positive for hepatitis C, usually in the first few days after a transplant. Generally, when part of a study, the drugs are paid for by the manufacturer or the institutions conducting the research.
When the drugs first hit the market at the end of 2013, a course of treatment cost $100,000. As more antivirals have become available, prices have fallen and coverage limits have eased for people with chronic hepatitis C. The average net price for a round of hep C antiviral therapy is now $25,167, according to SSR Health, part of SSR LLC, a boutique investment research firm.
Outside of those trials, transplant surgeons say they’ve sought — and often obtained — insurance coverage for the drugs. Durand said the move is cost-effective because the drugs cost less than ongoing dialysis for kidney failure or mechanical heart assist devices.
Researchers are split on whether there’s enough evidence to take the procedure out of the realm of scientific study.
“It isn’t the standard of care today, but it’s going in that direction,” said Durand.
Others advise caution until long-term results can be seen.
While the first 20 patients at Hopkins and Penn who received kidneys in a published study were all cured of hep C, “if we had 100 patients, or 200, then we would get a better sense as to whether the cure rate is 100 percent,” said Penn’s Reese.
The heart transplant program at Vanderbilt University Medical Center in Nashville has transplanted 42 non-infected patients with hearts exposed to hep C, and continues to follow them. Dr. Ashish Shah, the program’s director, noted that some people with untreated or long-term hepatitis C have a higher incidence of coronary artery disease.
“We’ll have to watch that,” he said, but noted that many patients with severe heart failure would otherwise die waiting for a transplant. “It’s reasonable to think that risks [of accepting an organ from a hepatitis-infected donor] are far lower.”
Jay Fuentes, a 45-year-old registered nurse in Quakertown, Pa., agreed to participate in the study at Penn in hopes of getting a transplant more quickly after his kidneys failed in 2017.
“It seemed like a no-brainer to me,” said Fuentes. “If I was in the first group where it had never been tried before, I might have hesitated.”
He tested positive for hepatitis C shortly after the surgery and took the antiviral drugs for 90 days. He said he no longer tests positive and has gotten back into performing in local theater with his children.
“I have a whole new lease on life,” said Fuentes.